Osseointegration
Contact Information
Osseointegration at Mass General
Yawkey Center for Outpatient Care
55 Fruit Street, Suite 3B
Boston,
MA
02114
Progam Administrator: Irene Kelley
Phone: 617-643-4947
Email: ikelley@mgh.harvard.edu
What is osseointegration?
Osseointegration is a term referring to the installation of a bone-anchored prosthetic limb following amputation. Your surgeon will surgically insert a metal implant (a titanium screw) into the bone of the residual limb. This implant extends through the skin, allowing direct external attachment to a prosthetic limb.
Currently, osseointegration is approved for patients with an above-the-knee amputation where a socket prosthesis may not work properly. Osseointegration at Mass General requires the expertise of our multidisciplinary team, which includes and plastic surgeons, prosthetists and rehab specialists. Our surgeons are some of the few clinicians offering this treatment in New England, and we are the only hospital in Massachusetts performing this surgery.
If you want more information about osseointegration, or wonder if you might be a candidate, call our office: 617-643-4947.
What are the benefits of an osseointegration implant?
The benefits of the osseointegration implant system are:
- Increased range of motion and limb strength
- Improved ability to sit comfortably
- A more natural gait
- Increased awareness of limb positioning and sense of feel through the prosthesis (proprioception)
- Faster putting on (donning) and taking off (doffing) of prothesis
- Increased duration of prosthetic wear time
- Improved quality of life
- The elimination of prosthesis-socket-related problems such as chafing and sores, sweating, pain, pressure and malfunction of the socket
- Eliminated need for prosthesis socket revision due to weight fluctuation
Frequently asked questions
Is osseointegration an option for all patients who have had amputations?
Currently, osseointegration implants are only FDA-approved for individuals aged 16 to 65 who have had above-the-knee (transfemoral) amputations and have a very small residual lower extremity. Your doctor may recommend you try a socket prosthesis at first, but the related issues of perspiration, skin irritation, ulcerations, and pain may lead you to explore other prosthesis options. Your doctor will review your particular case, including your femur bone density and integrity, and discuss with you whether or not osseointegration is a viable option.
This technology is not limited to cancer patients and is intended for any patient who meets the criteria above. These implants are intended for any patient who has undergone above-the-knee amputation and has a residual lower extremity that is too small to allow for the effective use of a socket prosthesis. However, osseointegration is not recommended for patients with a history of bone infection, also known as osteomyelitis. Patients with active bone infections, residual bone less than 8 cm in length, and less than 2 mm thickness of cortical bone are not eligible for this surgery. As part of your preoperative evaluation, our team will perform a thin-cut computed tomography (CT) scan of your residual lower extremity, in addition to radiographs, to accurately measure these parameters.
How should I prepare for osseointegration surgery?
Before your surgery, you will be assessed at the Interdisciplinary Care for Amputees Network (ICAN) Clinic. At this clinic, you will have the opportunity to learn about osseointegration surgery and the roles of orthopaedic and plastic surgery in the procedure. Addtionally, you will meet with a prosthetist and physical therapist. You may also receive counseling on nutritional optimization, smoking cessation and rehabilitation after surgery.
What is recovery like after osseointegration surgery?
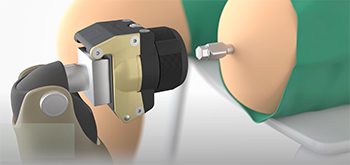
Osseointegrated implants consist of two main components: a fixture for anchoring and a skin-penetrating device known as the abutment. The fixture is surgically placed within the medullary canal of the remaining femoral bone. After a healing period of approximately three months, the abutment is connected to the fixture. Finally, the prosthesis is directly attached to the external part of the abutment.
After the second stage of the procedure, postoperative rehabilitation entails a standardized protocol with gradually increased levels of prothesis testing. Full weight-bearing with the definitive prosthesis is typically allowed immediately after the second stage with a series of prosthetics of different length, first a short one and then progressing to the final one.
Regular follow-up appointments are recommended, and typically include clinical examinations, mechanical assessments, and X-ray evaluations to ensure optimal outcomes and address any potential issues.
How long does the process of osseointegration take?
Osseointegration surgery involves two stages, and usually there is a three-month gap between the two procedures. The entire process takes four to six months, including the three-month waiting period between the stages, and leads to unencumbered walking (full ambulation).
How long does the implant last? Is it permanent?
Limb reconstruction through osseointegration surgery is intended to be a long-lasting solution. This durable and permanent treatment only requires further attention if you experience a bone fracture or infection in the area where the fixture is anchored, or aseptic loosening, which is a type of implant loosening not caused by infection.
What is the success rate of osseointegration?

The osseointegration system for transfemoral amputees has shown promising long-term outcomes in various studies. Over a ten-year period, patients reported significant improvements in prosthetic use, mobility, and physical function compared to before treatment. Our team is currently conducting a long-term study on patient-reported and functional outcomes following transfemoral osseointegration surgery, which will continue to inform our approach to amputation and prosthetics.
Are there risks or complications associated with osseointegration implant surgery following transfemoral amputation?
Complications associated with osseointegration surgery include concerns regarding mechanical complications, especially in individuals with higher activity levels, as well as rare complications related to superficial and deep infections that may require revision surgery. Your doctor will review your prosthesis options with you, including the pros and cons of osseointegration surgery as you explore your prosthesis options.
Is osseointegration surgery covered by insurance?
Yes, however, pre-approval is required, and many insurers require patients to try a standard socket prosthesis before they approve alternative options like osseointegration.
Osseointegration team members
-
![]()
Santiago Lozano-Calderon, MD, PhD
- Orthopaedic Oncology Surgeon
- Acting Director, Musculoskeletal Oncology Fellowship Program
- Associate Professor of Orthopaedic Surgery, Harvard Medical School
-
![]()
- Associate Professor of Surgery
- Program Director, Harvard Plastic Surgery Residency Program
- Associate Program Director, MGH Hand Surgery Fellowship
-
![]()
- Plastic and Reconstructive Surgery
- Department of Surgery
-
![]()
- Nurse Practitioner; Doctor of Nursing; Clinical Director, Ortho Oncology; Director, Ortho APPs
-
![]()
- Nurse Practitioner
-
![]()
- Physician Assistant, Department of Plastic & Reconstructive Surgery
Learn more about osseointegration
If you have questions about osseointegration or want more information, call our team.






