Patient Story2 Minute ReadJun | 10 | 2024
Kelli's Story: Mobile ECMO

Kelli Shaw, 34, believes in happy endings.
On June 9, 2024, the Bedford, New Hampshire mother of three celebrated her 10-year wedding anniversary with a vow renewal ceremony. It is a milestone she nearly did not live to see following a medical emergency less than a year ago.
“I had a routine hysterectomy the Friday before Thanksgiving in 2023,” says Kelli Shaw. “A few days later, I started to feel sick. My husband drove me to a local hospital with a terrible stomachache – and I went downhill fast,” she says.
Kelli Shaw was battling strep bacteremia and toxic shock syndrome. Her heart and lungs rapidly began to fail.
“She was in and out of consciousness, put on a breathing tube, and coded twice,” says her husband, Corey Shaw. “A doctor came out and explained the situation was dire. He asked for consent to consult with a colleague he knew at Mass General.”
Jerome Crowley, MD, of the MGH Heart Center Intensive Care Unit and Department of Anesthesia, Critical Care and Pain Medicine, boarded a Boston MedFlight helicopter with his team and a mobile Extra Corporeal Membrane Oxygenation (ECMO) machine. The ECMO treatment is used in patients experiencing life-threatening heart and lung failure, working to temporarily replace the function of the patient’s compromised organs so the body can heal.

“Mobile ECMO is relatively new – we began using it in 2020,” says Crowley. “In extreme cases when someone is too unstable to be moved and unlikely to survive without the expertise of a hospital like Mass General, the machine allows us to go to them. We have been able to grow this life saving program thanks to the support from the departments of Cardiac Surgery, Anesthesia and the perfusion team.”
For the Shaws, the MGH team was a welcome sight.
“I remember feeling utter shock, then knowing Dr. Crowley was landing in the chopper and seeing him burst through the doors to see my wife,” says Corey Shaw. “It was clear he knew what he was doing, and he was going to get the situation under control.”
Once stabilized, Kelli Shaw was transported to Mass General’s main campus where she continued the ECMO treatment for three days. She spent six weeks at MGH overall and was released to a rehabilitation facility the day before Christmas.
“The clinical team were calling her the ‘Christmas Miracle!’” Corey Shaw says.
Crowley credits the many clinical team members who were instrumental in ensuring a positive outcome, including Thor Sunt, MD, chief, MGH Cardiac Surgery; David D’Alessandro, MD, surgical director, Heart Transplantation and Ventricular Assist Devices; Eriberto Michel, MD, adult cardiac surgeon, MGH Cardiac Surgery; Kenneth Shelton, MD, chief, Division of Critical Care, Department of Anesthesia, Critical Care and Pain Medicine; Seun Johnson-Akeju, MD, anesthetist-in-chief; Joseph Catricala, MS, cardiovascular perfusionist; Kenneth Shann, director, Perfusion Services; and Nikolaos Zacharias, MD, vascular surgeon, Division of Vascular and Endovascular Surgery.
“Kelli made phenomenal progress thanks to a collaborative, multidisciplinary effort from Nursing, Physical Therapy, Respiratory Therapy, the Heart Center ICU team and Vascular Surgery,” says Crowley.
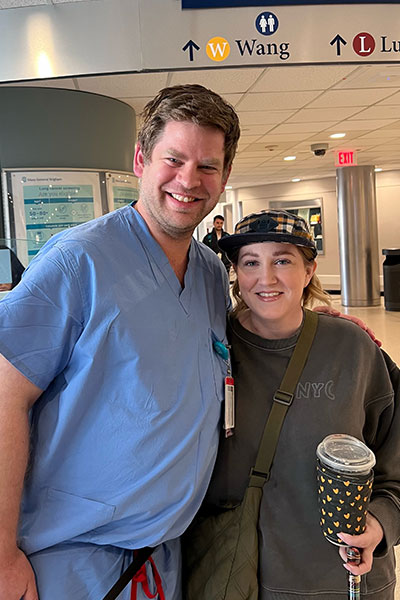
After her release, Kelli Shaw returned home in a wheelchair, then transitioned to a walker and then to a cane. She began planning the vow renewal celebration during her recovery as a way to look forward to something positive. Kelli Shaw also planned to personally share her appreciation with Crowley – and was able to do so during a recent visit to MGH.
“I can’t say enough about the entire Mass General team,” says Kelli Shaw. “It felt like a full circle moment: I was able to look at Dr. Crowley and thank him for saving my life, while standing on my own two feet.”
