George A. “Doc” Lopez, MD Lab for Regenerative Cell Therapy
Contact Information
The George A. “Doc” Lopez, MD Laboratory for Regenerative Cell Therapy
White 536, Massachusetts General Hospital
55 Fruit Street
Boston,
MA
02114
Contact Us
Bin Song, MD, PhD
bsong@mgh.harvard.edu
617-724-2673
Support Our Work
Sarah Gaylord
sgaylord@mgh.harvard.edu
617-797-5766
Explore This Laboratory
Overview
The George A. “Doc” Lopez, MD Laboratory for Regenerative Cell Therapy is situated within the Department of Neurosurgery at Massachusetts General Hospital and is led by Bin Song, MD, PhD, scientific director, and Jeffrey Schweitzer, MD, PhD, clinical director. The mission of the laboratory is to pioneer innovative methods for treating Parkinson’s disease and related degenerative disorders of the nervous system at the cellular level.
Our focus involves utilizing state-of-the-art tools for cellular reprogramming, gene editing, and directed differentiation of stem cell products. In addition to a cutting-edge cell and molecular neurobiology research laboratory, the Lopez Laboratory includes a self-contained Current Good Manufacturing Practice (cGMP) facility, specifically designed to exceed FDA standards of quality and safety for producing clinical-grade cell products for early-phase clinical trials. This unique integration of research and qualified controlled areas creates a conducive environment for pioneering translational research.
The laboratory's primary focus is on cellular therapies for Parkinson’s disease, and ongoing research projects include the refinement of reprogramming techniques for induced pluripotent stem cells, the development of novel differentiation protocols for generating dopaminergic neurons, and the exploration of technological innovations to enhance the survival of stem cell-derived grafts.
What is regenerative cell therapy?
Many neurodegenerative diseases involve the loss of specific cell types. This loss can occur due to a variety of underlying causes such as genetic, environmental, or both. Although medicines can substitute some of the functions of the lost cells, the substitution is incomplete and imperfect at best, has many side effects, and does not prevent progression of the disease. Similarly, current surgical therapies such as deep brain stimulation also treats just the symptoms and carry a different set of risks and limitations. While the concept of replacing cells lost in Parkinson’s disease originated decades ago, modern molecular biological, genetic, and stem cell techniques have opened many new avenues to safely and effectively overcome barriers to progress in this field. Replacing the lost cells carries the potential of more closely approximating a true cure, with more durable benefit and fewer side effects.
By further adopting the precision or personalized medicine approach, cellular replacement can achieve the optimum treatment for each patient. Advances in genetics and neuroscience give us the tools to develop novel therapies, while big data resources and machine learning help identify those at risk and facilitate more effective prevention or early intervention.
The idea behind precision medicine is to move beyond a one-size-fits-all approach by accounting for our individual differences in biology, environment, and lifestyle to develop more targeted and effective approaches to diagnosis, treatment, and prevention. We have already witnessed significant benefits from precision medicine, such as the development of targeted treatments for cancer and heart disease, along with novel methods for predicting an individual’s risk of these and other diseases. We now have an opportunity to bring precision medicine to the field of cell therapy for degenerative diseases of the brain.
Fundamental, unresolved questions persist in our ability to apply cell therapy in this manner:
- Are all patients with Parkinson's disease candidates for cell therapy using their own skin or blood cells as a tissue source, or does this only work for some?
- What is the best, safest, and most cost efficient method or methods for creating “working banks” of stem cells, and for differentiating them into the desired cell type?
- What are the best surgical techniques to help the replacement cells survive in the brain?
- Can we correct the molecular pathology in the transplanted cells that caused the disease in the patient?
- How does the outcome of such treatment compare to other therapies for Parkinson's disease? Can different forms of therapy be combined?
Our laboratory is committed to uncovering the answers to these and other questions for the advancement of cell therapies and the improvement of patient outcomes.
Research Focus
The Lopez Lab focuses on these key strategic areas:
hiPSC reprogramming
- The key to using autologous cell sources, or any reprogrammed cell source, is to create pluripotent stem cells safely as well as maintain pluripotency without epigenetic memory. The lab is actively researching improved methods to accomplish these goals.
- Exploring the differences amongst different cell sources such as fibroblasts or blood cells for safety and efficacy
- Combining reprogramming with gene editing may be a way to remove harmful mutations that underlie degenerative diseases while reducing time, cost, and risks inherent in multiple separate processes
Dopaminergic Differentiation of Pluripotent Cells
- Developing improved methods to promote uniform differentiation into the desired specific cell type, using small molecules where possible
- Validating potential dopaminergic cell transplantation products for authentic functionality in vitro prior to transplantation
- Identifying reliable markers of dopaminergic efficacy to permit verification and purification of desired cell lines
Improved Surgical Techniques
- Current surgical methods for transplantation of cell products into the brain result in the death of the some of the desired cells. The lab is actively researching the multiple causes of this cell loss
- Developing improved surgical methods and devices to overcome this obstacle
New models applicable to translational product development:
- Generally used animal Parkinson's disease models involve administration of toxins and are both etiologically and histopathologically different from the spontaneous human disease. Development of models that more closely approximate patient conditions will improve our understanding and ability to treat neurodegenerative disease
- Leverage large-scale genomic studies to identify the genetic basis of “sporadic” Parkinson's disease to determine if accessible mutations can be isolated and corrected for this majority population
- Use state-of-the art tools--including functional genomics and stem cell biology--to identify useful biomarkers and uncover mechanisms linking genes to disease
Education and Training
- A major role of the Lopez Lab will be the recruitment and training of graduate and post-graduate students
- Opportunities for interdisciplinary and cross-institutional collaboration will be actively developed
Our Research
- Jeon J, Cha, Y, Hong, YJ, Lee IH, Jang H, Ko S, Naumenko S, Kim M, Ryu HL, Shrestha Z, Lee N, Park TY, Park H, Kim SH, Yoon KJ, Song B, Schweitzer JS, Herrington TM, Kong SW, Carter B, Leblanc P, Kim KS. Pre-clinical safety and efficacy of human induced pluripotent stem cell-derived products for autologous cell therapy in Parkinson's disease. Cell Stem Cell 2025 Feb 6:S1934-5909(25)00006-2.
- Park TY, Jeon J, Lee N, Kim J, Song B, Kim JH, Lee SK, Liu D, Cha Y, Kim M, Leblanc P, Herrington TM, Carter BS, Schweitzer JS, Kim KS. Co-transplantation of autologous Treg cells in a cell therapy for Parkinson's disease. Nature. 2023; 619(7970):606-615.
- Xue J, Wu YF, Bao YT, Zhao ML, Li FZ, Sun J, Sun YM, Wang J, Chen L, Mao Y, Schweitzer JS, Song B. Clinical Considerations in Parkinson’s Disease Cell Therapy. Ageing Res. Rev. 2023; 83:101792.
- Schweitzer JS, Song B, Herrington TM, Park T-Y, Lee N, Ko S, Jeon J, Cha Y, Kim K, Li Q, Henchcliffe C, Kaplitt M, Neff C, Rapalino O, Seo H, Lee I-H, Kim J, Kim T, Petsko GA, Ritz J, Cohen BM, Kong SW, Leblanc P, Carter BS, Kim KS. Personalized iPSC-derived Dopamine Progenitor Cells for Parkinson’s Disease. N Eng J Med. 2020; 382:1926-1932.
- Song B, Cha Y, Ko S, Jeon J, Lee N, Seo H, Park KJ, Lee IH, Lopes C, Feitosa M, Luna MJ, Jung JH, Kim J, Hwang D, Cohen BM, Teicher MH, Leblanc P, Carter BS, Kordower JH, Bolshakov VY, Kong SW, Schweitzer JS, Kim KS. Human autologous iPSC-derived dopaminergic progenitors restore motor function in Parkinson’s disease models. J. Clin. Invest. 2020; 130:904-920.
- Schweitzer JS, Song B, Leblanc PR, Feitosa M, Carter BS, Kim KS. Columnar Injection for intracerebral Cell therapy. Oper Neurosurg (Hagerstown). 2020; 18:321-328.
Clinical Trial
The Lopez Laboratory is supporting clinical trial NCT06687837, Treating Parkinson's Disease Through Transplantation of Autologous Stem Cell-Derived Dopaminergic Neurons, which is currently enrolling participants. More information about the trial can be found on clinicaltrials.gov.
Our Team

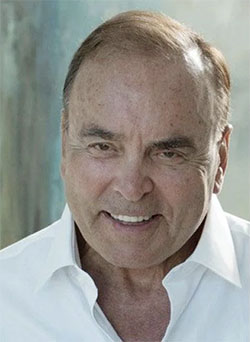
Jeffrey Schweitzer, MD, PhD
Clinical/Translational Director
Dr. Schweitzer is an Assistant Professor in the Department of Neurosurgery and brings over three decades of extensive experience in the surgical treatment of Parkinson’s disease and other movement disorders. Notably, he is the lead author of the first reported use in humans of autologous stem cell therapy to treat Parkinson’s disease, as reported in the New England Journal of Medicine. Dr. Schweitzer has published extensively in fields ranging from developmental cell biology to basic neurophysiology.

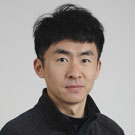
Bin Song, MD, PhD
Scientific Director
Dr. Song, scientific director, received her doctoral and postdoctoral training in Neuroscience, molecular and stem cell biology at Sun Yat Sen University, China and in the Molecular Neurobiology Laboratory at McLean Hospital’s at Harvard Medical School. Dr Song is first author of the preclinical report underlying the first use in humans of autologous stem cell therapy, published in the Journal of Clinical Investigation. She has also contributed significantly to the scientific community through dozens of key papers in the fields of neurodegeneration and stem cell biology.

Tatyana Matveeva, PhD
Senior cGMP Cell Production Manager
Dr. Matveeva holds a PhD in Cognitive and Brain Sciences from the University of Minnesota. She completed a post-doctoral fellowship at the Tschida Social Neuroscience Laboratory of Cornell University studying circuit-level mechanisms of social behavior and an additional post-doctoral fellowship at the New England Complex Systems Institute focused on public health and policy.

Tanner Boyd
Research Technician II
Tanner Boyd received his bachelor’s degree in neuroscience at Boston University in 2022. Before he joined the Lopez Llab in 2024, he worked in a lab in the Department of Neurology studying with mouse and cellular models to investigate roles of tau aggregation in the propagation of Alzheimer’s disease.
Chen Qiu, PhD
Postdoctoral Research Fellow
Chen holds a PhD in Cell Biology from Zhejiang University, China in 2023, mainly focusing on tissue engineering for spinal cord injury. After he joined the Lopez Lab in 2024, he is focused on different types of Parkinson’s disease animal models and exploringe new cell therapeutic approaches for Parkinson’s disease.

Aryan Galani
Research Technologist
Aryan received his bachelor's in biochemistry and molecular biology from Rhodes College in 2021. Before joining the Lopez lab, he was a manufacturing lead at Moderna, producing mRNA-based vaccines for phase I, II, and III clinical trials. He also worked as a research assistant at the Molecular Immunotherapeutics Research (MIR) lab at Rhodes College, where he engineered protein antivirals for a SARS-CoV-2 therapeutic.
#1 Research Hospital in America
Mass General is the #1 research hospital in America, with a large percentage of that dedicated to Neuro-related diseases.
Advances in Motion
Advances in Motion provides health care professionals with information about the latest breakthroughs, research & clinical advances from Mass General.
Parkinson's Disease Stem Cell Therapy
Learn about our recent developments in stem-cell therapy, research and news.
Department of Neurosurgery
The Department of Neurosurgery at Massachusetts General Hospital provides a complete range of surgical services for the diagnosis, surgical treatment and rehabilitation of neurologic disorders of the brain and spine.
