Vocal Hyperfunction Clinical Research Center
Contact Information
Vocal Hyperfunction Clinical Research Center
Center for Laryngeal Surgery and Voice Rehabilitation
One Bowdoin Square, 11th Floor
Boston,
MA
02114
Phone: 617-643-2466
Email: sederosa@mgh.harvard.edu
News and Events
November 15, 2023: The NIDCD-funded (P50) Vocal Hyperfunction Clinical Research Center (VHCRC) will be hosting a day-long meeting at the Massachusetts General Hospital the day before the ASHA Convention in Boston on Wednesday, November 15, 2023, 8:00 am–5:00 pm ET. The morning will be devoted to progress reports for the four Center projects, and we will have five invited speakers in the afternoon. The overall goal is to increase the exchange of information with outside groups that are doing research in related areas. The public is also invited to attend in person or virtually. Please RSVP to Sarah DeRosa (sederosa@mgh.harvard.edu) as in-person space is limited.
Explore the Center
About the Center

The Vocal Hyperfunction Clinical Research Center (VHCRC) at Massachusetts General Hospital is a comprehensive, multi-institutional research program that brings together an interdisciplinary team of investigators with various specialties to study hyperfunctional voice disorders. The VHCRC is led by Robert Hillman, PhD, CCC-SLP, research director and co-director of the Mass General Voice Center. The central theme of the VHCRC is that clinical management of vocal hyperfunction can be significantly improved by attaining a better understanding of the multiple causative factors and associated disordered physiological processes associated with these disorders and then translating this knowledge into new, more effective methods for prevention, diagnosis and treatment.
The center’s scope of research in vocal hyperfunction is unprecedented, especially with respect to the integration of many types of data (e.g., behavioral, sensorimotor, environmental, psychological/emotional and biomechanical data) on a large scale, across multiple institutions and areas of expertise.
About the Condition
Vocal hyperfunction refers to excessive or unbalanced activity of the perilaryngeal muscles (muscles connected to the voice box) during voice production. It is associated with the most prevalent types of voice disorders including those that arise from repeated trauma to vocal cord tissue (for example, nodules and polyps) and the occurrence of vocal deterioration in the absence of an identified medical cause (commonly called muscle tension dysphonia).
Scientific Premise
Multiple factors are believed to cause and maintain the disorders linked to vocal hyperfunction. The most important mechanisms include:
- Anatomical/Physiological
- Behavioral
- Biomechanical
- Emotional
- Environmental
- Psychological
- Sensorimotor
The VHCRC’s interdisciplinary research program focuses on understanding the fundamental relationships between these factors and the different manifestations of vocal hyperfunction. This is being accomplished in four major research projects led by Dr. Hillman, Cara Stepp, PhD, Matías Zañartu, PhD, Jarrad Van Stan, PhD, and a technology and data science core led by Daryush Mehta, PhD. They employ an innovative combination of laboratory studies of sensorimotor and physiological mechanisms, including the impact of psychological stress; neural network modeling of voice motor control; computational and physical modeling of phonatory mechanisms; and the use of ambulatory biosensors to investigate the potential differential impact on vocal function of daily voice use, psychological stress and environmental noise in patients with vocal hyperfunction and well-matched normal controls. Use of ambulatory biofeedback as a treatment strategy is also being assessed.
Goals
- To better delineate the etiological and pathophysiological mechanisms that underlie the range of voice disorders associated with vocal hyperfunction
- To develop more specific and accurate classification or phenotyping of vocal hyperfunction based on solid scientific evidence of disparate underlying etiological and pathophysiological mechanisms
- To use the new information about mechanisms of vocal hyperfunction to develop and test new clinical methods to improve the prevention, differential diagnosis, and targeted behavioral treatment of hyperfunctional voice disorders
Vocal Hyperfunction Theoretical Framework (PDF)
Acknowledgments: The VHCRC is supported by funding from the National Institutes of Health National Institute on Deafness and Other Communication Disorders through Grant P50 DC015446, which was renewed for another 5-year cycle on April 17, 2023. Website content is solely the responsibility of the investigators and does not necessarily represent the official views of the National Institutes of Health.
Active Research Projects
The below four research projects focus on investigating mechanisms that are hypothesized to play primary roles in causing and/or maintaining vocal hyperfunction (VH). Expand each title to learn more.
Identifying physical and behavioral factors and mechanisms to improve detection and phenotyping of vocal hyperfunction
Multiple Principal Investigators: Robert E. Hillman, PhD, CCC-SLP, and Daryush D. Mehta, PhD, Mass General
This project continues to elucidate multiple factors/mechanisms that are assumed to play important roles in causing and maintaining hyperfunctional voice disorders using a combination of data from ambulatory voice monitoring and other important sources: reflux status, personality, vocal reactivity to environmental sound levels, responses to voice therapy and ambulatory biofeedback, assessment of auditory-motor deficits, and model-generated estimates of phonatory physiological parameters that are difficult/impossible to measure clinically. Research during this second grant cycle will focus on the interrelated goals of further improving the detection of VH and identifying clinically meaningful subgroups (phenotypes) within the broad categories of VH. A combination of advanced statistical and machine learning approaches will be applied to our growing comprehensive/multidimensional voice database to optimize the discovery of VH subgroups based on differences in objective measures of daily (ambulatory) vocal behavior and phonatory pathophysiology. The subgroups will be further differentiated by additional measures that reflect deeper insights into pathophysiological mechanisms (e.g., intrinsic laryngeal muscle activation levels, vocal fold collision pressure, etc.) and potential predisposing factors (e.g., personality, reflux, etc.).
Sensorimotor mechanisms of vocal hyperfunction
Principal Investigator: Cara E. Stepp, PhD, Boston University
This project uses classic model-driven experimental approaches from speech motor control research to test hypotheses concerning the potential role that disordered sensorimotor mechanisms play in VH. Our central hypothesis, supported by our recent findings, is that auditory-motor function is impaired in some individuals with VH: we found impairments in speakers’ auditory acuity to differences in recordings of their own voice fundamental frequency and their adaptive responses to artificial shifts in their own voice fundamental frequency. We propose to further elucidate the etiologic role of disrupted auditory-motor function in VH and to evaluate measures of auditory-motor function that have clinical applicability. This understanding could allow for assessments that are sensitive to each patient, allowing personalized therapy approaches based on underlying mechanisms.
Modeling biomechanical, aero-acoustic, and auditory-motor control mechanisms of vocal hyperfunction
Principal Investigator: Matías Zañartu, PhD, Universidad Técnica Federico Santa María
This project develops and uses physical and numerical modeling (including subject-specific models) to provide unique insights into the underlying biomechanical, aero-acoustic, and auditory-motor control mechanisms that contribute to the pathophysiology of VH, providing direct links between model outputs and real clinical data with direct application to the ambulatory assessment of vocal function. This project seeks to determine the underlying physical and neurophysiological mechanisms associated with VH, with the goal of identifying triggering mechanisms and differentiating cause from reaction in these disorders. In addition, subject-specific model representations will provide access to additional measures and insights from the available data that will help to elucidate the etiology and pathophysiology of VH.
Use of ambulatory biofeedback to improve behavioral treatment of vocal hyperfunction
Principal Investigator: Jarrad H. Van Stan, PhD, CCC-SLP, Mass General
VH is the most commonly treated class of voice disorders by speech-language pathologists and voice therapy is the primary curative treatment. Patients and clinicians report that generalizing improved voicing into daily life is the most significant barrier to successful therapy. In this project, we will test if extending biofeedback into the patient’s daily life using ambulatory voice monitoring will significantly improve generalization during therapy and if individual patient factors, like how easily they can modify their voice and engagement during therapy, moderate the effects of the biofeedback.
Past Reseach Projects
April 1, 2017–March 31, 2023
The following three research projects were pursued during the first funding cycle. Expand each title to learn more.
Use of ambulatory biosensors to improve the differential diagnosis and treatment of vocal hyperfunction
Principal Investigator: Robert E. Hillman, PhD, CCC-SLP, Mass General
This project uses an innovative combination of ambulatory biosensors, clinical and laboratory studies, and tracking of treatment-related effects to gain new insights into behavioral (daily voice use), environmental (noise levels), emotional (psychological stress/arousal), and physiological (phonatory function) factors related to the etiology and pathophysiology of VH. Researchers will assess the assumed role of emotional stress in eliciting a differential VH response in patients with hyperfunctional voice disorders and normal controls. In a secondary analysis, the team will examine the hypothesized impact of personality and psychological predisposition (trait theory) in modulating the vocal/VH response to emotional stress by having participants complete personality inventories. A major thrust of this project will involve testing hypotheses about the differential impact of VH on the phonatory physiology (biomechanics) associated with phonotraumatic VH (e.g., nodules) and nonphonotraumatic VH (e.g., muscle tension dysphonia). This will also include investigating the potential modulating impact on VH of environmental noise levels (Lombard Effect – increasing vocal SPL) and the presence of nodules (e.g., testing hypotheses related to the need for post-surgical voice therapy to reduce persistent/residual phonotraumatic VH). Special emphasis will be placed on testing biomechanics-based hypotheses related to the role of collision forces in phonotraumatic VH. Use of ambulatory biofeedback as a treatment strategy will also be assessed.
Sensorimotor mechanisms of vocal hyperfunction
Principal Investigator: Cara E. Stepp, PhD, Boston University
This project uses classic model-driven experimental approaches from speech motor control research to test hypotheses concerning the potential role that disordered sensorimotor mechanisms play in VH. Auditory-motor integration for feedforward and feedback control are examined. These studies include the potential impact that voice therapy might have in reducing such deficits by triggering neuroplastic central nervous system changes. This project will rely on ambulatory measures that are being further refined in Project 1 to assess pre- and post-treatment changes in daily vocal function.
Modeling biomechanical and aero-acoustic mechanisms of vocal hyperfunction
Principal Investigator: Matías Zañartu, PhD, Universidad Técnica Federico Santa María
This project develops and uses physical and numerical modeling (including subject-specific models) to provide unique insights into the underlying biomechanical, aero-acoustic, and muscle activation mechanisms that contribute to the pathophysiology of VH, providing direct links between model outputs and real clinical data with direct application to the ambulatory assessment of vocal function. This important fundamental work closely links/integrates with Projects 1 and 2 by providing unique insights into these mechanisms that cannot be obtained with current approaches and, in the case of Project 1, extending or improving ambulatory assessment of daily vocal function for clinical evaluation and treatment (biofeedback).
Publications
Expand the below categories to view a sampling of our work, all of which is supported by clinical research center funding.
Publications
- Espinoza VM, Zañartu M, Van Stan JH, Mehta DD, Hillman RE (2017). Glottal aerodynamic measures in women with phonotraumatic and nonphonotraumatic vocal hyperfunction. Journal of Speech, Language, and Hearing Research, 60(8):2159–2169. PMCID: PMC5829799. link
- Van Stan JH, Park S-W, Jarvis M, Mehta DD, Hillman RE, Sternad D (2017). Measuring vocal motor skill with a virtual voice-controlled slingshot. The Journal of the Acoustical Society of America, 142(3):1199–1212. PMCID: PMC5648563. link
- Borsky M, Mehta DD, Van Stan JH, Gudnason J (2017). Modal and non-modal voice quality classification using acoustic and electroglottographic features. IEEE/ACM Transactions on Audio, Speech, and Language Processing, 25(12):2281–2291. PMCID: PMC7971071. link
- Galindo GE, Peterson SD, Erath BD, Castro C, Hillman RE, Zañartu M (2017). Modeling the pathophysiology of phonotraumatic vocal hyperfunction with a triangular glottal model of the vocal folds. Journal of Speech, Language, and Hearing Research, 60(9):2452–2471. PMCID: PMC5831616. link
- Van Stan JH, Maffei M, Masson MLV, Mehta DD, Burns JA, Hillman RE (2017). Self-ratings of vocal status in daily life: Reliability and validity for patients with vocal hyperfunction and a normative group. American Journal of Speech-Language Pathology, 26(4):1167–1177. PMCID: PMC5945061. link
- Cortés JP, Espinoza VM, Ghassemi M, Mehta DD, Van Stan JH, Hillman RE, Guttag JV, Zañartu M (2018). Ambulatory assessment of phonotraumatic vocal hyperfunction using glottal airflow measures estimated from neck-surface acceleration. PLoS One, 13(12):e0209017. PMCID: PMC6301575. link
- Gonzalez Ortiz JJ, Guttag J, Hillman RE, Mehta DD, Van Stan JH, Ghassemi M (2019). Learning from few subjects in the presence of large amounts of ambulatory data. Proceedings of Machine Learning Research, 106:704–720.PMCID: PMC8456782. link
- Brockmann-Bauser M, Van Stan JH, Carvalho Sampaio M, Bohlender JE, Hillman RE, Mehta DD (2021). Effects of vocal intensity and fundamental frequency on cepstral peak prominence in patients with voice disorders and vocally healthy controls. Journal of Voice, 35(3): 411–417. PMCID: PMC7295673. link
- Ciccarelli G, Mehta DD, Ortiz A, Van Stan JH, Toles L, Marks K, Hillman RE, Quatieri T. (2019). Correlating an ambulatory voice measure to electrodermal activity in patients with vocal hyperfunction. Proceedings of the 16th International Conference on Wearable and Implantable Body Sensor Networks, 2019:18850875. PMCID: PMC8278873. link
- Deliyski DD, Shishkov M, Mehta DD, Ghasemzadeh H, Bouma B, Zañartu M, de Alarcon A, Hillman RE (2021). Laser-calibrated system for transnasal fiberoptic laryngeal high-speed videoendoscopy. Journal of Voice, 35(1):122–128. PMCID: PMC6995434. link
- Deng JJ, Hadwin PJ, Peterson SD (2019). The effect of high-speed videoendoscopy configuration on reduced-order model parameter estimates by Bayesian inference. The Journal of the Acoustical Society of America, 146(2):1492–1492. PMCID: PMC6715443. link
- Díaz-Cádiz ME, Peterson SD, Galindo GE, Espinoza VM, Motie-Shirazi M, Erath BD, Zañartu M (2019). Estimating vocal fold contact pressure from raw laryngeal high-speed videoendoscopy using a Hertz contact model. Applied Sciences, 9(11):2384. PMCID: PMC8279006. link
- Erath BD, Peterson SD, Weiland KS, Plesniak MW, Zañartu M (2019). An acoustic source model for asymmetric intraglottal flow with application to reduced-order models of the vocal folds. PLoS One, 14(7):e0219914. PMCID: PMC6657872. link
- Hadwin PJ, Motie-Shirazi M, Erath BD, Peterson SD (2019). Bayesian inference of vocal fold material properties from glottal area waveforms using a 2D finite element model. Applied Sciences, 9(13):2735. PMCID: PMC8153513. link
- Heller Murray ES, Hseu AF, Nuss RC, Harvey Woodnorth G, Stepp CE (2019). Vocal pitch discrimination in children with and without vocal fold nodules. Applied Sciences, 9(15):3042. PMCID: PMC6910133. link
- Heller Murray ES, Lupiani AA, Kolin KR, Segina RK, Stepp CE (2019). Pitch shifting with the commercially available Eventide Eclipse: Intended and unintended changes to the speech signal. Journal of Speech, Language, and Hearing Research, 62(7):2270–2279. PMCID: PMC6808353. link
- Manriquez R, Peterson SD, Prado P, Orio P, Galindo GE, Zañartu M (2019). Neurophysiological muscle activation scheme for controlling vocal fold models. IEEE Transactions on Neural Systems and Rehabilitation Engineering, 27(5):1043–1052. PMCID: PMC6557719. link
- Mehta DD, Espinoza VM, Van Stan JH, Zañartu M, Hillman RE (2019). The difference between first and second harmonic amplitudes correlates between glottal airflow and neck-surface accelerometer signals during phonation. The Journal of the Acoustical Society of America, 145(5):EL386–EL392. PMCID: PMC6520097. link
- Mehta DD, Kobler JB, Zeitels SM, Zañartu M, Erath BD, Motie-Shirazi M, Peterson SD, Petrillo RH, Hillman RE (2019). Toward development of a vocal fold contact pressure probe: Bench-top validation of a dual-sensor probe using excised human larynx models. Applied Sciences, 9(20):4360. PMCID: PMC8171492. link
- Motie-Shirazi M, Zañartu M, Peterson SD, Mehta DD, Kobler JB, Hillman RE, Erath BD (2019). Toward development of a vocal fold contact pressure probe: Sensor characterization and validation using synthetic vocal fold models. Applied Sciences, 9(15):3002. PMCID: PMC7202565. link
- Murton O, Shattuck-Hufnagel S, Choi J-Y, Mehta DD (2019). Identifying a creak probability threshold for an irregular pitch period detection algorithm. The Journal of the Acoustical Society of America, 145(5):EL379–EL385. PMCID: PMC6520096. link
- Ortiz AJ, Toles LE, Marks KL, Capobianco S, Mehta, DD, Hillman RE, Van Stan JH (2019). Automatic speech and singing classification in ambulatory recordings for normal and disordered voices. The Journal of the Acoustical Society of America, 146(1):EL22–EL27. PMCID: PMC6624122. link
- Park Y, Perkell JS, Matthies ML, Stepp CE (2019). Categorization in the perception of breathy voice quality and its relation to voice production in healthy speakers. Journal of Speech, Language, and Hearing Research, 62(10):3655–3666. PMCID: PMC7201331. link
- Prado-Gutierrez P, Martínez-Montes E, Weinstein A, Zañartu M (2019). Estimation of auditory steady-state responses based on the averaging of independent EEG epochs. PLoS One, 14(1):e0206018. PMCID: PMC6345467. link
- Marks KL, Lin JZ, Fox AB, Toles LE, Mehta DD (2019). Impact of nonmodal phonation on estimates of subglottal pressure from neck-surface acceleration in healthy speakers. Journal of Speech, Language, and Hearing Research, 62(9):3339–3358. PMCID: PMC6808343. link
- Alzamendi GA, Manríquez R, Hadwin PJ, Deng JJ, Peterson SD, Erath BD, Mehta DD, Hillman RE, Zañartu M (2020). Bayesian estimation of vocal function measures using laryngeal high-speed videoendoscopy and glottal airflow estimates: An in vivo case study. The Journal of the Acoustical Society of America, 147(5):EL434–EL439. PMCID: PMC7480079. link
- Ghasemzadeh H, Deliyski DD, Ford DS, Kobler JB, Hillman RE, Mehta DD (2020). Method for vertical calibration of laser-projection transnasal fiberoptic high-speed videoendoscopy. Journal of Voice, 34(6):847–861. PMCID: PMC6883161. link
- Espinoza VM, Mehta DD, Van Stan JH, Hillman RE, Zañartu M (2020). Glottal aerodynamics estimated from neck-surface vibration in women with phonotraumatic and nonphonotraumatic vocal hyperfunction. Journal of Speech, Language, and Hearing Research, 63(9):2861–2869. PMCID: PMC7890221. link
- Heller Murray ES, Segina RK, Woodnorth GH, Stepp CE (2020). Relative fundamental frequency in children with and without vocal fold nodules. Journal of Speech, Language, and Hearing Research, 63(2):361–371. PMCID: PMC7210445. link
- Hillman RE, Stepp CE, Van Stan JH, Zañartu M, Mehta DD (2020). An updated theoretical framework for vocal hyperfunction. American Journal of Speech-Language Pathology, 29(4):2254–2260. PMCID: PMC8740570. link
- Kearney E, Nieto-Castañón A, Weerathunge HR, Falsini R, Daliri A, Abur D, Ballard KJ, Chang SE, Chao SC, Heller Murray ES, Scott TL, Guenther FH (2020). A simple 3-parameter model for examining adaptation in speech and voice production. Frontiers in Psychology, 10:2995. PMCID: PMC6985569. link
- Lin JZ, Espinoza VM, Marks KL, Zañartu M, Mehta DD (2020). Improved subglottal pressure estimation from neck-surface vibration in healthy speakers producing non-modal phonation. IEEE Journal of Selected Topics in Signal Processing, 14(2):449–460. PMCID: PMC8168553. link
- Marks KL, Lin JZ, Burns JA, Hron TA, Hillman RE, Mehta DD (2020). Estimation of subglottal pressure from neck surface vibration in patients with voice disorders. Journal of Speech, Language, and Hearing Research, 63(7):2202–2218. PMCID: PMC7838842. link
- McKenna VS, Hylkema JA, Tardif MC, Stepp CE (2020). Voice onset time in individuals with hyperfunctional voice disorders: Evidence for disordered vocal motor control. Journal of Speech, Language, and Hearing Research, 63(2):405-420. PMCID: PMC7210440. link
- Mora LA, Ramirez H, Yuz JI, Le Gorec Y, Zañartu M (2021). Energy-based fluid–structure model of the vocal folds. IMA Journal of Mathematical Control and Information, 38(2):466–492. PMCID: PMC8210679. link
- Heller Murray ES, Stepp CE (2020). Relationships between vocal pitch perception and production: A developmental perspective. Scientific Reports, 10(1):3912. PMCID: PMC7054315. link
- Lester-Smith RA, Daliri A, Enos N, Abur D, Lupiani AA, Letcher S, Stepp CE (2020). The relation of articulatory and vocal auditory-motor control in typical speakers. Journal of Speech, Language, and Hearing Research, 63(11):3628–3642. PMCID: PMC8582832. link
- Martínez-Montes E, García-Puente Y, Zañartu M, Prado-Gutiérrez P (2020). Chirp analyzer for estimating amplitude and latency of steady-state auditory envelope following responses. IEEE Transactions on Neural Systems and Rehabilitation Engineering, 28(12):2744–2753. PMCID: PMC7920094. link
- Murton O, Hillman R, Mehta D (2020). Cepstral peak prominence values for clinical voice evaluation. American Journal of Speech-Language Pathology, 29(3):1596–1607. PMCID: PMC7893528. link
- Toles LE, Ortiz AJ, Marks KL, Mehta DD, Van Stan JH, Hillman RE (2022). Amount and characteristics of speaking and singing voice use in vocally healthy female college student singers during a typical week. Journal of Voice, 36(2):203–211. PMCID: PMC7680342. links
- Tracy LF, Segina RK, Cadiz MD, Stepp CE (2020). The impact of communication modality on voice production. Journal of Speech, Language, and Hearing Research, 63(9):2913–2920. PMCID: PMC7890225. link
- Van Stan JH, Mehta DD, Ortiz AJ, Burns JA, Marks KL, Toles LE, Stadelman-Cohen T, Krusemark C, Muise J, Hron T, Zeitels SM, Fox AB, Hillman RE (2020). Changes in a Daily Phonotrauma Index after laryngeal surgery and voice therapy: Implications for the role of daily voice use in the etiology and pathophysiology of phonotraumatic vocal hyperfunction. Journal of Speech, Language, and Hearing Research, 63(12):3934–3944. PMCID: PMC8608140. link
- Van Stan JH, Mehta DD, Ortiz AJ, Burns JA, Toles LE, Marks KL, Vangel M, Hron T, Zeitels S, Hillman RE (2020). Differences in weeklong ambulatory vocal behavior between female patients with phonotraumatic lesions and matched controls. Journal of Speech, Language, and Hearing Research, 63(2):372–384. PMCID: PMC7210443. link
- Weerathunge HR, Abur D, Enos NM, Brown KM, Stepp CE (2020). Auditory-motor perturbations of voice fundamental frequency: Feedback delay and amplification. Journal of Speech, Language, and Hearing Research, 63(9):2846–2860. PMCID: PMC7890227. link
- Whittico TH, Ortiz AJ, Marks KL, Toles LE, Van Stan JH, Hillman RE, Mehta DD (2020). Ambulatory monitoring of Lombard-related vocal characteristics in vocally healthy female speakers. The Journal of the Acoustical Society of America, 147(6):EL552–EL558. PMCID: PMC7316514. link
- Groll MD, Vojtech JM, Hablani S, Mehta DD, Buckley DP, Noordzij JP, Stepp CE (2022). Automated relative fundamental frequency algorithms for use with neck-surface accelerometer signals. Journal of Voice, 36(2):156–169. PMCID: PMC7790853. link
- Ghasemzadeh H, Deliyski DD (2020). Non-linear image distortions in flexible fiberoptic endoscopes and their effects on calibrated horizontal measurements using high-speed videoendoscopy. Journal of Voice: in press, S0892-1997(20)30331-3 PMCID: PMC7969477. link
- Kridgen S, Hillman RE, Stadelman-Cohen T, Zeitels S, Burns JA, Hron T, Krusemark C, Muise J, Van Stan JH (2021). Patient-reported factors associated with the onset of hyperfunctional voice disorders. Annals of Otology, Rhinology & Laryngology, 130(4):389–394. PMCID: PMC7940573. link
- Toles LE, Ortiz AJ, Marks KL, Burns JA, Hron T, Van Stan J, Mehta DD, Hillman RE (2020). Differences between female singers with phonotrauma and vocally healthy matched controls in singing and speaking voice use during 1 week of ambulatory monitoring. American Journal of Speech-Language Pathology, 30(1):199–209. PMCID: PMC8740583. link
- Ghasemzadeh H, Deliyski DD, Hillman RE, Mehta DD (2021). Method for horizontal calibration of laser-projection transnasal fiberoptic high-speed videoendoscopy. Applied Sciences, 11(2):822. PMCID: PMC7899170. link
- Van Stan JH, Ortiz AJ, Cortés JP, Marks KL, Toles LE, Mehta DD, Burns JA, Hron T, Stadelman-Cohen T, Krusemark C, Muise J, Fox-Galalis AB, Nudelman C, Zeitels SM, Hillman RE (2021). Differences in daily voice use measures between female patients with nonphonotraumatic vocal hyperfunction and matched controls. Journal of Speech, Language, and Hearing Research, 64(5):1457–1470. PMCID: PMC8608188. link
- Van Stan JH, Ortiz AJ, Marks KL, Toles LE, Mehta DD, Burns JA, Hron T, Stadelman-Cohen T, Krusemark C, Muise J, Fox AB, Nudelman C, Zeitels SM, Hillman RE (2021). Changes in the Daily Phonotrauma Index following the use of voice therapy as the sole treatment for phonotraumatic vocal hyperfunction in females. Journal of Speech, Language, and Hearing Research, 64(9):3446–3455. PMCID: PMC8642084. link
- Marks KL, Verdi A, Toles LE, Stipancic KL, Ortiz AJ, Hillman RE, Mehta DD (2021). Psychometric analysis of an ecological vocal effort scale in individuals with and without vocal hyperfunction during activities of daily living. American Journal of Speech-Language Pathology, 30(6):2589–2604. PMCID: PMC9132024. link
- Toles LE, Roy N, Sogg S, Marks KL, Ortiz AJ, Fox AB, Mehta DD, Hillman RE (2021). Relationships among personality, daily speaking voice use, and phonotrauma in adult female singers. Journal of Speech, Language, and Hearing Research, 64(12):4580–4598. PMCID: PMC9150681. link
- Mehta DD, Kobler JB, Zeitels SM, Zañartu M, Ibarra EJ, Alzamendi GA, Manriquez R, Erath BD, Peterson SD, Petrillo RH, Hillman RE (2021). Direct measurement and modeling of intraglottal, subglottal, and vocal fold collision pressures during phonation in an individual with a hemilaryngectomy. Applied Sciences, 11(16):7256. PMCID: PMC9541559. link
- Ibarra EJ, Parra J, Alzamendi GA, Cortés JP, Espinoza VM, Mehta DD, Hillman RE, Zañartu M (2021). Estimation of subglottal pressure, vocal fold collision pressure, and intrinsic laryngeal muscle activation from neck-surface vibration using a neural network framework and a voice production model. Frontiers in Physiology, 12(732244):13 pages. PMCID: PMC8440844. link
- Van Stan JH, Ortiz AJ, Sternad D, Mehta DD, Huo C, Hillman RE (2021). Ambulatory voice biofeedback: Acquisition and retention of modified daily voice use in patients with phonotraumatic vocal hyperfunction. American Journal of Speech-Language Pathology, 31(1):409–418. PMCID: PMC9135013. link
- Van Stan JH, Park S-W, Jarvis M, Stemple J, Hillman RE, Sternad D (2021). Quantitative Assessment of Learning and Retention in Virtual Vocal Function Exercises. Journal of Speech, Language, and Hearing Research, 65(1): 1–15. PMCID: PMC8608156. link
- Kapsner-Smith MR, Díaz-Cádiz ME, Vojtech JM, Buckley DP, Mehta DD, Hillman RE, Tracy LF, Noordzij JP, Eadie TL, Stepp CE (2022). Clinical cutoff scores for acoustic indices of vocal hyperfunction that combine relative fundamental frequency and cepstral peak prominence. Journal of Speech, Language, and Hearing Research, 65(4):1349–1369. PMCID: PMC9499364. link
- Nudelman CJ, Ortiz AJ, Fox AB, Mehta DD, Hillman RE, Van Stan JH (2022). Daily Phonotrauma Index: An objective indicator of large differences in self-reported vocal status in the daily life of females with phonotraumatic vocal hyperfunction. American Journal of Speech-Language Pathology, 31(3):1412–1423. PMCID: PMC9567307. link
- Cler GJ, Perkell JS, Stepp CE (2021). Oral configurations during vowel nasalization in English. Speech Communication, 129:17–24. PMCID: PMC8492006. link
- Groll MD, Hablani S, Stepp CE (2021). The relationship between voice onset time and increases in vocal effort and fundamental frequency. Journal of Speech, Language, and Hearing Research, 64(4):1197–1209. PMCID: PMC8608153. link
- Serry MA, Stepp CE, Peterson SD (2021). Physics of phonation offset: Towards understanding relative fundamental frequency observations. The Journal of the Acoustical Society of America, 149(5):3654–3664. PMCID: PMC8163514. link
- Abur D, Subaciute A, Kapsner-Smith M, Segina RK, Tracy LF, Noordzij JP, Stepp, CE (2021). Impaired auditory discrimination and auditory-motor integration in hyperfunctional voice disorders. Scientific Reports, 11(1):13123. PMCID: PMC8222324. link
- Abur D, MacPherson MK, Shembel AC, Stepp CE (2021). Acoustic Measures of Voice and Physiologic Measures of Autonomic Arousal During Speech as a Function of Cognitive Load in Older Adults. Journal of Voice, 31(4):504.e1–504.e9. PMCID: PMC8310524. link
- Tomassi NE, Weerathunge HR, Cushman MR, Bohland JW, Stepp CE (2022). Assessing ecologically valid methods of auditory feedback measurement in individuals with typical speech. Journal of Speech, Language, and Hearing Research, 65(1):121–135. PMCID: PMC9153919. link
- Tomassi NE, Castro ME, Timmons Sund L, Díaz-Cádiz ME, Buckley DP, Stepp CE (2021). Effects of sidetone amplification on vocal function during telecommunication. Journal of Voice, S0892-1997(21)00124-7. PMCID: PMC8586047.. link
- Weerathunge HR, Alzamendi GA, Cler GJ, Guenther FH, Stepp CE, Zañartu M (2022). LaDIVA: A neurocomputational model providing laryngeal motor control for speech acquisition and production. PLoS Computational Biology, 18(6):e1010159. PMCID: PMC9258861. link
- Motie-Shirazi M, Zañartu M, Peterson SD, Erath BD (2021). Vocal fold dynamics in a synthetic self-oscillating model: Contact pressure and dissipated energy dose. Journal of the Acoustical Society of America, 150(2):1332–1345. PMCID: PMC8298101. link
- Hadwin PJ, Erath BD, Peterson SD (2021). The influence of flow model selection on finite element model parameter estimation using Bayesian inference. JASA Express Letters, 1(4): 045204. PMCID: PMC8182970. link
- Serry MA, Stepp CE, Peterson SD (2021). Physics of phonation offset: Towards understanding relative fundamental frequency observations. Journal of the Acoustical Society of America, 149(5):3654–3664. PMCID: PMC8163514. link
- Stewart ME, Erath BD (2021). Investigating blunt force trauma to the larynx: The role of inferior-superior vocal fold displacement on phonation. Journal of Biomechanics, 121; 110377. PMCID: PMC8127414. link
- Motie-Shirazi M, Zañartu M, Peterson SD, Erath BD (2021). Vocal fold dynamics in a synthetic self-oscillating model: Intraglottal aerodynamic pressure and energy. Journal of the Acoustical Society of America, 150(2):1332–1345. PMCID: PMC8387087. link
- Ghasemzadeh H, Deliyski DD, Hillman RE, Mehta DD. Framework for indirect spatial calibration of the horizontal plane of endoscopic laryngeal images. Journal of Voice 2022:in press. PMCID: PMC9249951. link
- Alzamendi GA, Peterson SD, Erath BD, Hillman RE, Zañartu M (2022). Triangular body-cover model of the vocal folds with coordinated activation of five intrinsic laryngeal muscles. Journal of the Acoustical Society of America, 151(1):17–30. PMCID: PMC8727069. link
- Cortés JP, Alzamendi GA, Weinstein AJ, Yuz GI, Espinoza VM, Mehta DD, Hillman RE, Zañartu M (2022). Kalman filter implementation of subglottal impedance-based inverse filtering to estimate glottal airflow during phonation. Applied Sciences, 12(1):401. PMCID: PMC9615581. link
- Deng J, Serry M, Zañartu M, Erath BD, Peterson SD (2022). Modeling the influence of COVID-19 protective measures on the mechanics of phonation. Journal of the Acoustical Society of America, 151(5):2987–2998. PMCID: PMC9068248. link
- Weerathunge HR, Tomassi NE, Stepp CE (2022). What can altered auditory feedback paradigms tell us about vocal motor control in individuals with voice disorders? Perspectives of the ASHA Special Interest Groups, 1–18. PMCID: PMC10312128. link
- Motie-Shirazi M, Peterson SD, Zañartu M, Mehta DD, Hillman RE, Erath BD (2022). Collision pressure and dissipated power dose in a self-oscillating silicone vocal fold model with a posterior glottal opening. Journal of Speech, Language, and Hearing Research, 65(8):2829–2845. PMCID: PMC9911124. link
- Castro C, Prado P, Espinoza VM, Testart A, Marfull D, Manríquez R, Stepp CE, Mehta DD, Hillman RE, Zañartu M (2022). Lombard effect in individuals with non-phonotraumatic vocal hyperfunction: Impact on acoustic, aerodynamic, and vocal fold vibratory parameters. Journal of Speech, Language, and Hearing Research, 65(8):2881–2895. PMCID: PMC9913286. link
- Toles LE, Seidman AY, Hillman RE, Mehta DD (2022). Clinical utility of the ratio of sound pressure level to subglottal pressure in patients surgically treated for phonotraumatic vocal fold lesions. Journal of Speech, Language, and Hearing Research, 65(8):2778–2788. PMCID: PMC9911101. link
- Cortés JP, Lin JZ, Marks KL, Espinoza VM, Ibarra EJ, Zañartu M, Hillman RE, Mehta DD. Ambulatory monitoring of subglottal pressure estimated from neck-surface vibration in individuals with and without voice disorders. Applied Sciences 2022;12(21):10692. PMCID: PMC9910342. link
- Groll MD, Peterson SD, Zañartu M, Vojtech JM, Stepp CE (2022). Empirical evaluation of the role of vocal fold collision on relative fundamental frequency in voicing offset. Journal of Voice, in press. PMCID: PMC10154433. link
- Motie-Shirazi M, Zañartu M, Peterson SD, Mehta DD, Hillman RE, Erath BD. Effect of nodule size and stiffness on phonation threshold and collision pressures in a synthetic hemilaryngeal vocal fold model. The Journal of the Acoustical Society of America 2023;153(1):654–664. PMCID: PMC9884154. link
- Bullock L, Toles LE, Hillman RE, Mehta DD. Acoustic-aerodynamic voice outcome ratios identify changes in vocal function following vocal fold medialization for unilateral vocal fold paralysis. Journal of Voice 2023:in press. PMID: 37068982. NIHMSID: NIHMS1883597. link
- Van Stan JH, Burns J, Hron T, Zeitels S, Panuganti BA, Purnell PR, Mehta DD, Hillman RE, Ghasemzadeh H. Detecting mild phonotrauma in daily life. Laryngoscope 2023:in press. PMID: 37194664. NIHMSID: NIHMS1901014. link
- Ghasemzadeh H, Azad AI, Deliyski DD. External validity of calibrated measurements from a laser-projection transnasal fiberoptic high-speed videoendoscopy system. Journal of Voice 2023:in press. PMCID: PMC9339040. link
- Serry M, Stepp CE, Peterson SD (2023). Exploring the mechanics of fundamental frequency variation during phonation onset. Biomechanics and Modeling in Mechanobiology, 22, 339–356. PMCID: PMC10369356. link
Conference Abstracts
- A. Testart, G. Galindo, C. Castro, M. Zañartu. “A new visual probabilistic assessment of vocal fold vibration”, The 12th International Conference on Advances in Quantitative Laryngology, Voice and Speech Research, Hong Kong, October 17-21, 2017.
- J. P. Cortés, M. Zañartu. “Ambulatory classification of patients with muscle tension dysphonia vs. control group”, The 12th International Conference on Advances in Quantitative Laryngology, Voice and Speech Research, Hong Kong, October 17-21, 2017.
- R. Manrıquez, S. D Peterson, P. Prado, P. Orio, M. Zañartu, “Laryngeal muscle activation noise for physiologically-based models of phonation”, The 12th International Conference on Advances in Quantitative Laryngology, Voice and Speech Research, Hong Kong, October 17-21, 2017.
- R. Manrıquez, S. D Peterson, P. Prado, P. Orio, M. Zañartu, “Modeling Laryngeal Muscle Activation Noise for Low-Order Physiological Based Speech Synthesis”, Proc. Interspeech 2017, pp 1378- 1382, Stockholm, Sweden, August 2017
- V. M. Espinoza, M. Zañartu, J. H. Van Stan, D. D. Mehta, and R. E. Hillman “Uncertainty of glottal airflow estimation during continuous speech using impedance-based inverse filtering of the neck-surface acceleration signal”, Fall 2017 meeting of the ASA, Boston, USA, June 25-29, 2017.
- Mehta D. D., Van Stan J. H., Masson M. L. V., Maffei M., Hillman R. E. Relating ambulatory voice measures with self-ratings of vocal fatigue in individuals with phonotraumatic vocal hyperfunction. Proceedings of the Acoustical Society of America 2017.
- Cortés J. P., Zañartu M., Mehta D. D., Van Stan J. H., Hillman R. E. Classification of patients with muscle tension dysphonia and matched-controls using ambulatory voice monitoring. Proceedings of the International Conference on Advances in Quantitative Laryngology, Voice and Speech Research 2017.
- Capobianco S., Ruggles R., Ortiz A. J., Mehta D. D., Hillman R. E., Van Stan J. H. Automatic classification of speech and singing during ambulatory voice monitoring using a neck-placed accelerometer. Proceedings of La Voce Artistica 2017.
- J.P. Cortes, V. M. Espinoza, M. Ghassemi, D. Mehta, J. Van Stan, R. Hillman, J. Guttag, M. Zañartu, “Using Aerodynamic Features and Their Uncertainty for the Ambulatory Assessment of Phonotraumatic Vocal Hyperfunction” IEEE International Conference on Biomedical and Health Informatics, March 4-7, 2018 in Las Vegas, NV.
- Brockmann-Bauser M., Van Stan J. H., Bohlender J. E., Mehta D. D. Acoustic-based cepstral peak prominence and spectral slope improve with increasing vocal intensity in women with and without voice disorders. Proceedings of the 12th Congress of the European Laryngological Society (ELS) 2018; London, England.
- Brockmann-Bauser M., Van Stan J. H., Bohlender JE, Mehta D. D. Effect of vocal intensity on cepstral peak prominence and spectral slope in women with and without voice disorders. Proceedings of the Voice Foundation Symposium 2018; Philadelphia, PA.
- Marks K. L. and Mehta D. D. Impact of non-modal phonation on estimates of subglottal pressure from neck-surface acceleration in healthy speakers. Proceedings of the Voice Foundation Symposium 2018; Philadelphia, PA.
- Van Stan J. H., Capobianco S., Ruggles R. K., Ortiz A. J., Toles L. E., Marks K. L., Hillman R. E., Mehta D. D. Ambulatory voice measures during singing and speech in patients with phonotraumatic vocal fold lesions compared to matched controls. Proceedings of the Voice Foundation Symposium 2018; Philadelphia, PA.
- Ghasemzadeh H., Naghibolhosseini M., Mehta D. D., Deliyski D. D. Machine-learning approach for automatic detection of calibrated laser light in transnasal flexible high-speed videoendoscopy. Proceedings of the Voice Foundation Symposium 2018; Philadelphia, PA.
- Deliyski D., Mehta D. D., Zañartu M., Shishkov M., Bouma B., de Alarcón A., Ghasemzadeh H., Hillman R. E. Laser-calibrated system for laryngeal transnasal flexible high-speed videoendoscopy. Proceedings of the Voice Foundation Symposium 2018; Philadelphia, PA.
- Brockmann-Bauser M., Van Stan J., Bohlender J. E., Mehta D. D. Spectral acoustic measures improve with increasing vocal intensity. Proceedings of the 29thth Congress of Union of the European Phoniatricians (UEP) 2018; Helsinki, Finland.
- P. Prado, C. Christian, A. Weinstein, L. Zepeda, M. Zañartu, “Cortical activation of healthy volunteers and muscle tension dysphonia (MTD) patients during Lombard Effect: an EEG study”, Joint meeting of the Chilean Societies of Biology, Genetics, Evolution, and Neuroscience, November 20-22, Puerto Varas, Chile, 2018.
- Hadwin, P. J. and Peterson, S. D., "Bayesian Inference of Tissue Properties from Glottal Area Waveforms Using a 2D Finite Element Model," 176th Meeting of the Acoustical Society of America, Victoria, BC, November 5-9, 2018.
- M. Diaz, M. Zañartu, C. Stepp, “How to construct your own high-speed flexible video endoscopy system for research and clinical applications”, The Fall Voice Conference 2018, October 25-27, Seattle, Washington, 2018.
- Park Y., Stepp C. E. “Do people who have breathier voices perceive breathiness differently?,” The Fall Voice Conference, Seattle, WA, October 25 – October 27, 2018. [poster presentation]
- Heller Murray E. S., Kolin K. R., Harvey Woodnorth G., Stepp C. E. “Relative Fundamental Frequency in Children With and Without Vocal Fold Nodules”, American Speech and Hearing Association (ASHA) Convention, Boston, MA, November 15-17, 2018. [podium presentation]
- V. Espinoza, D. Mehta, J. VanStan, R. E. Hillman, M. Zañartu, “Accelerometer-based aerodynamic measures for subjects with phonotraumatic hyperfunction: An in-laboratory study”, 11th International Conference on Voice Physiology and Biomechanics, August 1-3, 2018, East Lansing, Michigan.
- Heller Murray E.S., Lupiani A.A., Kolin K.R., Stepp C.E. “Accuracy of the commercially available Eventide Eclipse to perturb Auditory feedback of fundamental frequency”, 11th International Conference on Voice Physiology and Biomechanics, East Lansing, MI, August 1 – 3, 2018. [poster presentation]
- C. Castro, P. Prado, D. Marfull, A. Testart, A. Weinstein, L. Zepeda, V. Espinoza, M. Zañartu, “Lombard effect and muscle tension dysphonia: acoustic, aerodynamic, biomechanical and cortical changes”, 11th International Conference on Voice Physiology and Biomechanics, August 1-3, 2018, East Lansing, Michigan.
- J.P. Cortés, V. M. Espinoza, M. Ghassemi, D. Mehta, J. Van Stan, R. Hillman, J. Guttag, M. Zañartu, “Aerodynamic Ambulatory Assessment for Phonotraumatic Vocal Hyperfunction”, 11th International Conference on Voice Physiology and Biomechanics, August 1-3, 2018, East Lansing, Michigan.
- Deng, J., Hadwin, P. J. and Peterson, S. D., “The Influence of High-Speed Videoendoscopy Data Quality on Reduced-Order Model Parameters Estimated Using Bayesian Inference," 11th International Conference on Voice Physiology and Biomechanics, East Lansing, MI, August 1-3, 2018.
- M. Motie-Shirazi, B. D. Erath. “The effect of a posterior glottal gap on contact pressures in a synthetic self-oscillating vocal fold model,” 11th International Conference on Voice Physiology and Biomechanics, East Lansing, MI July 31-August 3, 2018.
- Mehta D., Kobler J., Zeitels S., Hillman R. In vivo probe for tracking intraglottal pressure, vocal fold collision, and subglottal pressure during phonation. Proceedings of the 11th International Conference on Voice Physiology and Biomechanics 2018; East Lansing, MI.
- Mehta D. D., Van Stan J. H., Hillman R. E. Toward objective ambulatory measures of vocal status in patients with vocal hyperfunction. Proceedings of the 11th International Conference on Voice Physiology and Biomechanics 2018; East Lansing, MI.
- Toles L., Ortiz A. J., Mehta D. D., Hillman R. E., Van Stan J. H. Speech and singing detection in ambulatory voice recordings in patients with phonotraumatic lesions and controls. Proceedings of the Annual Convention of the American Speech-Language-Hearing Association 2018; Boston, MA.
- Marks K, Lin J. Z., Mehta D. D. Estimating subglottal pressure from anterior neck-surface acceleration in patients with voice disorders. Proceedings of the Annual Convention of the American Speech-Language-Hearing Association 2018; Boston, MA.
- Hylkema J., McKenna V. S., Stepp C. E. “Voice Onset Time in Individuals with Hyperfunctional Voice Disorders”, American Speech and Hearing Association (ASHA) Convention, Boston, MA, November 15-17, 2018. [poster presentation]
- Mehta D. D., Whittico T. H., Ortiz A. J., Marks K. L., Toles L. E., Van Stan J. H., Hillman RE. Investigating ambulatory Lombard effects during the daily life of patients with phonotraumatic vocal hyperfunction. Proceedings of the Occupational Voice Symposium 2019; London, UK.
- Van Stan J. H., Stadelman-Cohn T., Muise J., Krusemark C., Ortiz A. J., Mehta D. D., Burns J. A., Hron T. A., Hillman R. E. Personalized ambulatory biofeedback for patients with vocal hyperfunction. Proceedings of the Occupational Voice Symposium 2019; London, UK.
- Ghasemzadeh H., Ford D. S., Deliyski D. D., Kobler J. B., Hillman R. E., Mehta D. D. Calibration method for laser-projection transnasal flexible high-speed videoendoscopy. Proceedings of the Voice Foundation Symposium 2019; Philadelphia, PA. Received Sataloff Award.
- Gabriel A. Alzamendi, Christian Castro Toro, Sean D. Peterson, Byron D. Erath, Matías Zañartu, “Modeling Modal, Breathy, and Pressed Voice Qualities: The Role of Intrinsic Laryngeal Muscle Activation”, 48th Voice Foundation Annual Symposium: Care of the Professional Voice, Philadelphia, Pennsylvania, May 29 - June 2, 2019.
- Juan Pablo Cortés, Víctor M. Espinoza, Christian Castro Toro, Rodrigo Manríquez Peralta, Alba Testart Tobar, Matías Zañartu, “Classification Performance of Paired Subjects with Vocal Hyperfunction in the Presence of Subglottal Inverse Filtering Uncertainties: Pilot Study under Laboratory Conditions”, 48th Voice Foundation Annual Symposium: Care of the Professional Voice, Philadelphia, Pennsylvania, May 29 - June 2, 2019.
- Pavel Prado, Álvaro Cavieres, Lucia Zepeda, Alejandro Weinstein, Matías Zañartu, Sonja Kotz, Wael El-Deredy, “Understanding Cortical Activation Associated with Corollary Discharge during Speech Production: The Role of Active and Passive Listening”, 48th Voice Foundation Annual Symposium: Care of the Professional Voice, Philadelphia, Pennsylvania, May 29 - June 2, 2019.
- Matías Zañartu, “Estimating Vocal Fold Contact Pressure In Vivo from Raw Laryngeal High-Speed Videoendoscopy using a Hertz Contact Model”, invited talk at the special session “Quantifying Vocal Fold Contact Pressure using Direct and Indirect Measurement Modalities”, 48th Voice Foundation Annual Symposium: Care of the Professional Voice, Philadelphia, Pennsylvania, May 29 - June 2, 2019.
- Sean D. Peterson “Quantifying Vocal Fold Contact Pressure through Bayesian Estimation of Reduced and High-Order Vocal Fold Models”, invited talk at the special session “Quantifying Vocal Fold Contact Pressure using Direct and Indirect Measurement Modalities”, 48th Voice Foundation Annual Symposium: Care of the Professional Voice, Philadelphia, Pennsylvania, May 29 - June 2, 2019.
- Byron D. Erath “Quantifying Uncertainty in Contact Pressure Measurements with Synthetic, Self-Oscillating Vocal Fold Models”, invited talk at the special session “Quantifying Vocal Fold Contact Pressure using Direct and Indirect Measurement Modalities”, 48th Voice Foundation Annual Symposium: Care of the Professional Voice, Philadelphia, Pennsylvania, May 29 - June 2, 2019.
- Daryush D. Mehta, “Validating Vocal Fold Contact Pressure Measurement using Excised Human Larynx Models”, invited talk at the special session “Quantifying Vocal Fold Contact Pressure using Direct and Indirect Measurement Modalities”, 48th Voice Foundation Annual Symposium: Care of the Professional Voice, Philadelphia, Pennsylvania, May 29 - June 2, 2019.
- Deliyski D. D., Ghasemzadeh H., Ford D. S., Mehta D. D., Shishkov M., Bouma B. E., Kobler J. B., Zanartu M., de Alarcon A., Hillman R. E. Laser-projection system and method for 3D calibrated laryngeal measurements using transnasal flexible high-speed videoendoscopy. Proceedings of the International Conference on Advances in Quantitative Laryngology, Voice and Speech Research 2019.
- Mehta D. D., Kobler J. B., Zañartu M., Erath B. D., Motie-Shirazi M., Peterson S. D., Petrillo R. H., Hillman R. E. Vocal fold collision pressure amplitude and timing in an excised hemilarynx setup with dual high-speed videoendoscopy. Proceedings of the International Conference on Advances in Quantitative Laryngology, Voice and Speech Research 2019.
- Van Stan J. H., Vangel M., Mehta D. D., Ortiz A. J., Toles L. E., Marks K. L., Hillman R. E. Differences in ambulatory vocal behavior between patients with phonotraumatic lesions and matched healthy controls. Proceedings of the International Conference on Advances in Quantitative Laryngology, Voice and Speech Research 2019.
- Cortés J. P., Alzamendi G. A., Weinstein A, Yuz J. I., Espinoza V. M., Mehta D. D., Van Stan J. H., Hillman R. E., Zañartu M. Uncertainty of ambulatory airflow estimates and its effect on the classification of phonotraumatic vocal hyperfunction. Proceedings of the International Conference on Advances in Quantitative Laryngology, Voice and Speech Research 2019.
- MotieShirazi M., Peterson S. D., Zañartu M., Mehta D. D., Kobler J. B., Hillman R. E., Erath B. D. Contact pressure and length as a function of posterior glottal area: Synthetic vocal fold investigations. Proceedings of the International Conference on Advances in Quantitative Laryngology, Voice and Speech Research 2019.
- Lin J. Z., Espinoza V. M., Zañartu M., Marks K. L., Mehta D. D. Accelerometer-based prediction of subglottal pressure in healthy speakers producing non-modal phonation. Proceedings of the International Conference on Advances in Quantitative Laryngology, Voice and Speech Research 2019.
- Espinoza V. M., Mehta D. D., Van Stan J..H , Hillman R. E., Zañartu M. Comparing accelerometer and oral airflow based aerodynamic measures in patients with vocal hyperfunction. Proceedings of the International Conference on Advances in Quantitative Laryngology, Voice and Speech Research 2019.
- Pavel Prado, Christian Castro, Alejandro Weinstein, Lucía Zepeda, Juan Mucarquer and Matías Zañartu,” Cortical Mechanisms Controlling the Speech Production During Lombard Effect: An EEG Study.”, The 13th International Conference on Advances in Quantitative Laryngology, Voice and Speech Research, Montreal, Quebec, Canada, June 2 - 4, 2019.
- Jonathan Deng, Paul Hadwin, Mohsen Motie-Shirazi, Byron Erath, Matías Zañartu And Sean Peterson,” Extracting Reduced-Order Model Parameters from High-Speed Video Of Silicone Vocal Folds Using A Gradient-Based Approach”, The 13th International Conference on Advances in Quantitative Laryngology, Voice and Speech Research, Montreal, Quebec, Canada, June 2 - 4, 2019.
- Paul Hadwin, Mohsen Motie-Shirazi, Byron Erath, Matías Zañartu And Sean Peterson,” Estimating Patient-Specific Contact Pressures Using A Finite Element Model”, The 13th International Conference on Advances in Quantitative Laryngology, Voice and Speech Research, Montreal, Quebec, Canada, June 2 - 4, 2019.
- Gabriel A. Alzamendi, Sean D. Peterson, Byron Erath And Matías Zañartu, “Updated Rules for Constructing A Triangular Body-Cover Model Of The Vocal Folds From Intrinsic Laryngeal Muscle Activation”, The 13th International Conference on Advances in Quantitative Laryngology, Voice and Speech Research, Montreal, Quebec, Canada, June 2 - 4, 2019.
- Gabriel Alzamendi, Sean Peterson, Byron Erath And Matías Zañartu, “On the Role Of Simultaneous Observations For A Bayesian Estimation Of Subglottal Pressure And Laryngeal Muscle Activation”, The 13th International Conference on Advances in Quantitative Laryngology, Voice and Speech Research, Montreal, Quebec, Canada, June 2 - 4, 2019.
- Heller Murray E. S., Hseu A., Nuss R., Harvey Woodnorth G., Stepp C. E. “Auditory acuity to fundamental frequency in children with and without vocal fold nodules”, The 13th International Conference on Advances in Quantitative Laryngology, Voice and Speech Research, Montreal, Quebec, June 2 – 4, 2019. [podium presentation]
- Aaron A, Ortiz AJ, Mehta D, Hillman R, Van Stan J. Ambulatory trends in objective voice measures associated with self-reported vocal status change for patients with vocal hyperfunction and matched controls. Proceedings of The Fall Voice Conference 2019; Dallax, TX.
- Marks KL, Toles LE, Mehta DD, Hillman RE. Psychometric analysis of the Singing Voice Handicap Index-10 in singers with vocal hyperfunction and healthy controls. Proceedings of The Fall Voice Conference 2019; Dallax, TX.
- Ghasemzadeh H, Deliyski DD, Hillman RE, Mehta DD. Accurate detection of spatially calibrating laser points during transnasal, fiberoptic, laryngeal high-speed videoendoscopy using support vector machine. Proceedings of The Acoustical Society of America 2019; San Diego, CA.
- Ghasemzadeh, H., Deliyski, D. D. (2020). Non-Linear Image Distortions in Flexible Fiberoptic Endoscopes and Their Effects on Laser-Calibrated Horizontal Measurements. The Voice Foundation’s 49th. Annual Symposium: Care of the Professional Voice, May 27-May 31.
- Ghasemzadeh, H., Deliyski, D. D. (2020). Horizontal Calibration for a Laser-Projection Transnasal Fiberoptic High-Speed Videoendoscopy. The Voice Foundation’s 49th. Annual Symposium: Care of the Professional Voice, May 27-May 31.
- Verdi A, Marks KL, Toles LE, Van Stan JH, Ortiz AJ, Hillman RE, Mehta DD. Ecological momentary assessment of vocal effort in patients with vocal hyperfunction. Proceedings of The Fall Voice Conference 2020; Virtual. Best Virtual Podium Presentation Award.
- Toles LE, Marks KL, Van Stan JH, Mehta DD, Hillman RE. The role of personality in the presence of phonotrauma in singers. Proceedings of The Fall Voice Conference 2020; Virtual.
- Brockmann-Bauser M, Van Stan JH, Sampaio MC, Bohlender JE, Hillman RE, Mehta DD. Effect of vocal intensity and fundamental frequency on cepstral peak prominence in women with and without voice disorders. Proceedings of the 12th International Conference on Voice Physiology and Biomechanics 2020; Grenoble, France (Virtual).
- Lin JZ, Espinoza VM, Marks KL, Zañartu M, Mehta DD. Improved subglottal pressure estimation from neck-surface vibration in patients with voice disorders. Proceedings of the 12th International Conference on Voice Physiology and Biomechanics 2020; Grenoble, France (Virtual).
- Mohsen Motie-Shirazi, Matias Zañartu, Sean D. Peterson, Byron D. Erath, “Compensation for a Posterior Glottal Opening Leads to Vocal Fold Trauma: Measurements of Contact Force as a Function of Aerodynamic and Kinematic Measures”, SB3C2020, Summer Biomechanics, Bioengineering and Biotransport Conference, June 17-20, 2020, Vail, CO, USA.
- Weerathunge H.R., Abur D., Enos N.M., Brown K., Stepp C.E. “Auditory-Motor Perturbations of Voice Fundamental Frequency: Effects of Feedback Delay and Amplification,” Conference on Motor Speech, Santa Barbara, CA, February 20-23, 2020. [poster presentation]
- Heller Murray E.S., Stepp C.E. “Vocal Pitch Perception and Production in Children and Adults,” Conference on Motor Speech, Santa Barbara, CA, February 20-23, 2020. [podium presentation]
- Kearney E., Smith D.J., Stepp C.E., Guenther F.H. “Contributions of Auditory and Somatosensory Feedback to Vocal Motor Control,” Conference on Motor Speech, Santa Barbara, CA, February 20-23, 2020. [poster presentation]
- Toles LE, Roy N, Sogg S, Marks KL, Ortiz AJ, Mehta DD, Hillman RE. Relationships between daily speaking voice use and personality in singers with healthy voices. Proceedings of the 14th International Conference on Advances in Quantitative Laryngology, Voice and Speech Research 2021; Bogotà, Colombia (Virtual).
- Marks KL, Verdi A, Toles LE, Stipancic KL, Ortiz AJ, Hillman RE, Mehta DD. Psychometric analysis of an ecological vocal effort scale in individuals with and without vocal hyperfunction during activities of daily living. Proceedings of the 14th International Conference on Advances in Quantitative Laryngology, Voice and Speech Research 2021; Bogotà, Colombia (Virtual).
- Cortés JP, Mehta DD, Ortiz AJ, Toles LE, Marks KL, Van Stan JH, Hillman RE. Relationships between the neck-surface acceleration parameters of the Daily Phonotrauma Index and glottal aerodynamic measures in vocally healthy females. Proceedings of the 14th International Conference on Advances in Quantitative Laryngology, Voice and Speech Research 2021; Bogotà, Colombia (Virtual).
- Van Stan JH, Ortiz AJ, Burns JA, Marks KL, Toles LE, Mehta DD, Hron T, Stadelman-Cohen T, Krusemark C, Muise J, Fox AB, Nudelman C, Zeitels SM, Hillman RE. Use of the Daily Phonotrauma Index (DPI) to quantify treatment-related changes in the daily voice use of patients with phonotrauma. Proceedings of the 14th International Conference on Advances in Quantitative Laryngology, Voice and Speech Research 2021; Bogotà, Colombia (Virtual).
- Ghasemzadeh H, Deliyski DD, Hillman RE, Mehta DD. Indirect spatial calibration of the horizontal plane of endoscopic laryngeal images: How to do it and what to look for. Proceedings of the 14th International Conference on Advances in Quantitative Laryngology, Voice and Speech Research 2021; Bogotà, Colombia (Virtual).
- Ciccarelli GA, Mehta DD, Ortiz AJ, Toles LE, Marks KL, Van Stan JH, Hillman RE, Quatieri TF. Ambulatory monitoring of the Lombard effect during the daily life of patients with hyperfunctional voice disorders. Proceedings of the 14th International Conference on Advances in Quantitative Laryngology, Voice and Speech Research 2021; Bogotà, Colombia (Virtual).
- G. A. Alzamendi, S. D. Peterson, B. D. Erath, M. Zañartu, “Investigating antagonistic muscle control in non-phonotraumatic vocal hyperfunction using a triangular body-cover model of the vocal folds”, 14th International Conference on Advances in Quantitative Laryngology, Voice and Speech Research, AQL 2021, June 7-10 2021, Online.
- R. Manríquez, V. M. Espinoza, C. Castro, J. P. Cortés, and M. Zañartu, Calibration Uncertainty of Impedance-based Inverse Filtering from Neck Surface Acceleration”, 14th International Conference on Advances in Quantitative Laryngology, Voice and Speech Research, AQL 2021, June 7-10 2021, Online.
- E. J. Ibarra, J. A. Parra, G. A. Alzamendi, J. P. Cortés, V. M. Espinoza, M. Zañartu, “A Machine Learning Framework for Estimating Subglottal Pressure during Running Speech from Glottal Airflow measures”, 14th International Conference on Advances in Quantitative Laryngology, Voice and Speech Research, AQL 2021, June 7-10 2021, Online.
- M. Motie-Shirazi, M. Zañartu, S. D. Peterson, B. D. Erath, “Influence of a posterior glottal opening on dissipated collision power: synthetic self-oscillating vocal fold investigations”, 14th International Conference on Advances in Quantitative Laryngology, Voice and Speech Research, AQL 2021, June 7-10 2021, Online.
- J. A. Parra, E. Ibarra, G. A. Alzamendi, J. P. Cortés, M. Zañartu. “Discovering Underlying Physical Parameters From Daily Phonotrauma Index Distributions using Monte Carlo Simulations of a Low-Dimensional Voice Production Model”, 14th International Conference on Advances in Quantitative Laryngology, Voice and Speech Research, AQL 2021, June 7-10 2021, Online.
- C. Castro, V. Espinoza, J. Pablo Cortes, P. Prado, M. Zañartu, “Lombard effect retention after noise removal in patients with phonotraumatic and non-phonotraumatic vocal hyperfunction”, 14th International Conference on Advances in Quantitative Laryngology, Voice and Speech Research, AQL 2021, June 7-10 2021, Online.
- M. D. Groll, S. D. Peterson, M. Zañartu, J. M. Vojtech, C. E. Stepp “Evaluating the relationship between relative fundamental frequency and the end of vocal fold collision in voicing offset”, 14th International Conference on Advances in Quantitative Laryngology, Voice and Speech Research, AQL 2021, June 7-10 2021, Online.
- Javier G. Fontanet, Juan I. Yuz, Matías Zañartu, “Parametric Identification of a Linear Time Invariant Model for a Subglottal System, 19th IFAC Symposium on System Identification, (SYSID 2021), July 13-16 2021, Online.
- M. Zañartu, D.D. Mehta, and R. E. Hillman, “Why is the clinical assessment of vocal aerodynamics relevant?”, The 2021 American Society of Thermal and Fluids Engineers (ASTFE) Conference, May 26-28, 2021.
- Mehta DD, Kobler JB, Zeitels SM, Petrillo RH, Hillman RE. In vivo measurement of intraglottal, subglottal, and vocal fold collision pressures in a hemilaryngectomy patient. Proceedings of the 14th International Conference on Advances in Quantitative Laryngology, Voice and Speech Research 2021; Bogotà, Colombia (Virtual).
- Emiro J. Ibarra, Jesús A. Parra, Gabriel A. Alzamendi, Juan P. Cortés, Víctor M. Espinoza, Matías Zañartu, “Método para la estimación de la función vocal usando un sensor de aceleración”, 77° Congreso Chileno de Otorrinolaringología 2021, 9-12 Noviembre 2021, online.
- J. Parra, M. Zañartu “Descubriendo parámetros físicos subyacentes a partir de las distribuciones ambulatorias diarias de un modelo matemático de voz”, 77° Congreso Chileno de Otorrinolaringología 2021, 9-12 Noviembre 2021, online.
- Emiro J. Ibarra, Jesús A. Parra, Gabriel A. Alzamendi, Juan P. Cortés, Víctor M. Espinoza, Matías Zañartu, “Método para la estimación de la función vocal usando un sensor de aceleración”, 77° Congreso Chileno de Otorrinolaringología 2021, 9-12 Noviembre 2021, online.
- J. Parra, M. Zañartu “Descubriendo parámetros físicos subyacentes a partir de las distribuciones ambulatorias diarias de un modelo matemático de voz”, 77° Congreso Chileno de Otorrinolaringología 2021, 9-12 Noviembre 2021, online.
- Mohsen Motie-Shirazi, Matías Zañartu, Sean Peterson, Byron Erath, “Fluid-structure energy exchange during phonation: investigation of dissipated collision energy by direct measurement of internal tissue velocity”, 74th Annual Meeting of the APS Division of Fluid Dynamics, November 21–23, 2021, Phoenix, Arizona.
- Mohsen Motie-Shirazi, Matías Zañartu, Sean Peterson, Byron Erath, “Fluid-structure energy exchange during phonation: investigation of dissipated collision energy by direct measurement of internal tissue velocity”, 74th Annual Meeting of the APS Division of Fluid Dynamics, November 21–23, 2021, Phoenix, Arizona.
- Marks KL, Toles LE, Houde L, Verdi A, Groll M, Hillman RE, Mehta DD. In-field relative fundamental frequency via neck-surface vibration in patients with vocal hyperfunction and vocally healthy controls. Proceedings of the Voice Foundation Symposium 2021; Philadelphia, PA (Virtual).
- Ghasemzadeh H, Deliyski DD, Hillman RE, Mehta DD, Verdolini Abbott K. Post-surgery changes in vocal fold closing velocity in patients with mass lesions. Proceedings of the Voice Foundation Symposium 2021; Philadelphia, PA (Virtual).
- Ghasemzadeh, H., Imani Azad, A., Deliyski, D. D. (2021). External Validity of Calibrated Measurements from a Laser-Projection Transnasal Fiberoptic High-Speed Videoendoscopy System. The Voice Foundation’s 50th. Annual Symposium: Care of the Professional Voice, June 2 – June 6.
- Seidman AY, Toles LE, Mehta DD. Clinical utility of vocal efficiency measures for voice disorder assessment. Proceedings of the American Speech-Language Hearing Association Convention 2021; Washington, DC.
- Abur D., Subaciute A., Kapsner-Smith M., Segina R.K., Tracy, L.F., Noordzij J.P., Stepp C.E. “Impaired auditory discrimination and sensorimotor integration in hyperfunctional voice disorders”, 14th International Conference on Advances in Quantitative Laryngology, Voice, and Speech Research, Virtual/Bogotá, Colombia, June 7-10, 2021. [podium presentation]
- Tomassi N.E., Castro M.E., Timmons Sund L., Diaz-Cadiz M.E., Buckley D.P., Stepp C.E. “Effects of sidetone amplification on vocal function during telecommunication”, 51st Annual Voice Foundation Symposium, Philadelphia, PA, June 1 – June 5, 2022. [podium presentation]
- Dahl K.L., Stepp C.E. “Effect of cognitive load on voice acoustics in individuals with hyperfunctional voice disorders,” 51st Annual Voice Foundation Symposium, Philadelphia, PA, June 1 – June 5, 2022. [poster presentation]
- Weerathunge H.R.†, Alzamendi G.A., Cler G.J., Guenther F.H., Stepp C.E., Zanartu M. “LaDIVA: A neurocomputational model providing laryngeal motor control for speech acquisition and production,” Conference on Motor Speech, Santa Barbara, CA, February 16, 2022. [podium presentation]
- Ghasemzadeh H, Hillman RE, Ortiz AJ, Van Stan J, Mehta DD. Discriminative power of ambulatory phonation and non-phonation behaviors to classify patients with phonotraumatic vocal hyperfunction and vocally healthy matched controls. Proceedings of the Voice Foundation Symposium 2022; Philadelphia, PA.
- Kapsner-Smith MR, Díaz-Cádiz ME, Vojtech JM, Buckley DP, Mehta DD, Hillman RE, Tracy LF, Noordzij JP, Eadie TL, Stepp CE. Clinical cutoff scores for acoustic indices of vocal hyperfunction that combine relative fundamental frequency and cepstral peak prominence. Proceedings of the Voice Foundation Symposium 2022; Philadelphia, PA. *Honorable Mention for David W. Brewer Award for Best Poster.
- Espinoza, VM, Cortés JP, Zañartu M, Alzamendi GA, Yuz JI, Mehta DD, Hillman RE. Modeling and estimation of neck-surface skin and subglottal systems with an ARMA-based model. Proceedings of the Voice Foundation Symposium 2022; Philadelphia, PA.
- Eastman SE, Hillman RE, Ghasemzadeh H, Mehta DD. Quantifying the occupational voice use of teachers. Proceedings of The Fall Voice Conference 2022; San Francisco, CA.
- Ghasemzadeh H, Hillman RE, Ortiz AJ, Van Stan JH, Mehta DD. Temporal quantification of voicing-resting patterns using ambulatory voice monitoring of patients with phonotraumatic vocal hyperfunction. Proceedings of the Annual Convention of the American Speech-Language-Hearing Association 2022; New Orleans, LA.
- J. P. Cortés, C. Castro, P. Prado, L. Zepeda, V. Espinoza, and M. Zañartu, “Exploring the Lombard effect in participants with non-phonotraumatic vocal hyperfunction using a simplified version of the DIVA model”, 51st Anniversary Symposium: Care of the Professional Voice, June 1 – 5, Philadelphia, PA, 2022.
- H. R. Weerathunge, G. A. Alzamendi, G. J. Cler, F. H. Guenther, C. E. Stepp, M. Zañartu “LaDIVA: A neurocomputational model providing laryngeal motor control for speech acquisition and production” Madonna Motor Speech Conference, Feb 17-20, 2022, Charleston, South Carolina.
- Ghasemzadeh H, Hillman RE, Ortiz AJ, Van Stan J, Mehta DD. Quantifying ambulatory voicing-resting behaviors reveals subtypes in patients with phonotraumatic vocal hyperfunction. Proceedings of the International Conference on Advances in Quantitative Laryngology, Voice and Speech Research 2023; Phoenix, AZ.
- Ghasemzadeh H, Hillman RE, Mehta DD. Giving statistical title back to machine learning: statistical power analysis and statistical model confidence of machine learning. Proceedings of the International Conference on Advances in Quantitative Laryngology, Voice and Speech Research 2023; Phoenix, AZ. *Conference Travel Award.
- Mehta DD, Guttag JV, Van Stan JH, Ghassemi M, Gonzalez Ortiz JJ, Ghasemzadeh H, Hillman RE. Enhancing clinical voice assessment with real-world, ambulatory monitoring of patients with voice disorders. Proceedings of the MIT-MGB AI Cures Conference 2023; Cambridge, MA.
- Van Stan JH, Burns J, Hron T, Zeitels S, Mehta D, Hillman RE, Ghasemzadeh H. Improved detection of mild phonotrauma in daily life. Proceedings of the Combined Otolaryngology Spring Meetings 2023; Boston, MA.
- Toles LE, Bullock PL, Hillman RE, Mehta DD. Acoustic-aerodynamic voice outcome ratios identify changes in vocal function following vocal fold medialization for unilateral vocal fold paralysis. Proceedings of the Annual Voice Foundation Symposium 2023; Philadelphia, PA.
- Ghasemzadeh H, Hillman RE, Espinoza VM, Ortiz AJ, Van Stan JH, Mehta DD. Subject-specific calibration of vocal fold dissipated power detects phonotrauma. Proceedings of the Annual Voice Foundation Symposium 2023; Philadelphia, PA.
- Ghasemzadeh H, Hillman RE, Ortiz AJ, Van Stan JH, Mehta DD. Phonotraumatic vocal hyperfunction manifests differently based on ambulatory monitoring of speaking versus singing. Proceedings of the Annual Voice Foundation Symposium 2023; Philadelphia, PA.
- E. Ibarra, G. A. Alzamendi, M. Zañartu, “Estimating the biomechanics of vocal function from glottal airflow measures using constrained extended Kalman filter and body cover model of the vocal folds”, Proceedings of the Annual Voice Foundation Symposium 2023; Philadelphia, PA.
- J. Martinez, M. Zañartu, “Comparative Analysis of Intrinsic Muscle Activation of the Larynx Using the EMG Decomposition Method in Different Phonatory Tasks. A Preliminary Study”, Proceedings of the Annual Voice Foundation Symposium 2023; Philadelphia, PA.
- J. Parra, BS, G. Alzamendi, M. Zañartu, “Nodule Approximation in a Triangular Shaped Vocal Fold Model“, Proceedings of the Annual Voice Foundation Symposium 2023; Philadelphia, PA.
- Aaron A., Volk K., Abur D., Stepp C.E. “The relationship between pitch discrimination and fundamental frequency variation: effects of singing status and vocal hyperfunction” The Fall Voice Conference, San Francisco, CA, October 6, 2023. [podium presentation]
Group Members
ADMINISTRATIVE CORE (LEAD: MASS GENERAL)
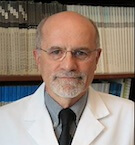 Robert Hillman, PhD, CCC-SLP
Robert Hillman, PhD, CCC-SLP
Director, Vocal Hyperfunction Clinical Research Center
Co-Director and Research Director, Mass General Voice Center
Professor of Surgery, Harvard Medical School
Director of Research Programs, MGH Institute of Health Professions
 Sarah DeRosa, MA
Sarah DeRosa, MA
Administrator Coordinator for Research and Speech-Language Pathology, Mass General Voice Center
TECHNOLOGY AND DATA SCIENCE CORE (LEAD: MASS GENERAL)
 Daryush Mehta, PhD
Daryush Mehta, PhD
Principal Investigator, Technology and Data Science Core, Vocal Hyperfunction Clinical Research Center
Director, Voice Science and Technology Laboratory, Mass General Voice Center
Associate Investigator, Mass General
Associate Professor of Surgery, Harvard Medical School
Adjunct Associate Professor, MGH Institute of Health Professions
Director of Student Affairs, Harvard Speech and Hearing Bioscience Technology Program
 Dimitar Deliyski, PhD
Dimitar Deliyski, PhD
MSU Foundation Professor and Department Chair, Michigan State University
 Jennifer Fellman
Jennifer Fellman
MS Student, Speech-Language Pathology, MGH Institute of Health Professions
 Laura Fishman
Laura Fishman
MS Student, Speech-Language Pathology, MGH Institute of Health Professions
 Annie B. Fox, PhD
Annie B. Fox, PhD
Associate Professor, MGH Institute of Health Professions
 Hamzeh Ghasemzadeh, PhD
Hamzeh Ghasemzadeh, PhD
Postdoctoral Research Fellow, Mass General Voice Center
Research Fellow in Surgery, Harvard Medical School
 Anatoly Goldstein, PhD
Anatoly Goldstein, PhD
Computer Systems Coordinator, Mass General Voice Center
 John Guttag, PhD
John Guttag, PhD
Dugald C. Jackson Professor of Computer Science and Electrical Engineering, Massachusetts Institute of Technology
 Ben Kevelson
Ben Kevelson
Research Engineer, Mass General Voice Center
 Katherine Matton, MSE
Katherine Matton, MSE
PhD Student, Electrical Engineering and Computer Science, MIT
 Andrew J. Ortiz, MS
Andrew J. Ortiz, MS
Research Engineer, Mass General Voice Center
 Rob Petit
Rob Petit
Software Developer, Consultant
 Samara Smith
Samara Smith
MS Student, Speech-Language Pathology, MGH Institute of Health Professions
 David Viggiano
David Viggiano
Software Developer, Consultant
 Zilan Zhu
Zilan Zhu
MS Student, Speech-Language Pathology, MGH Institute of Health Professions
PROJECT 1 (LEAD: MASS GENERAL)
 Robert Hillman, PhD, CCC-SLP
Robert Hillman, PhD, CCC-SLP
Director, Vocal Hyperfunction Clinical Research Center; Principal Investigator, Project 1
Co-Director and Research Director, Mass General Voice Center
Professor of Surgery, Harvard Medical School
Director of Research Programs, MGH Institute of Health Professions
 Daryush Mehta, PhD
Daryush Mehta, PhD
Principal Investigator, Project 1, Vocal Hyperfunction Clinical Research Center
Director, Voice Science and Technology Laboratory, Mass General Voice Center
Associate Investigator, Mass General
Associate Professor of Surgery, Harvard Medical School
Adjunct Associate Professor, MGH Institute of Health Professions
Director of Student Affairs, Harvard Speech and Hearing Bioscience Technology Program

Jarrad Van Stan, PhD, CCC-SLP
Research Speech-Language Pathologist, Mass General Voice Center
Assistant Professor in Surgery, Harvard Medical School
Adjunct Assistant Professor, MGH Institute of Health Professions
 Steven Zeitels, MD, FACS
Steven Zeitels, MD, FACS
Director of the Mass General Voice Center
Eugene B. Casey Professor of Laryngeal Surgery, Harvard Medical School
 Ahsan Cheema, MS
Ahsan Cheema, MS
PhD Student, Speech and Hearing Bioscience and Technology, Harvard University
 Grace Chow, BS
Grace Chow, BS
Clinical Research Coordinator, Boston Medical Center
 Jameson Cooper, MS, CCC-SLP
Jameson Cooper, MS, CCC-SLP
Research Speech-Language Pathologist, Mass General Voice Center
 Anna Frazier, BS
Anna Frazier, BS
PhD Student, Speech and Hearing Bioscience and Technology, Harvard University
 Hamzeh Ghasemzadeh, PhD
Hamzeh Ghasemzadeh, PhD
Postdoctoral Research Fellow, Mass General Voice Center
Research Fellow in Surgery, Harvard Medical School
 Amy Gottlieb, MS-CF-SLP
Amy Gottlieb, MS-CF-SLP
Speech-Language Pathologist, Boston Medical Center
 James Heaton, PhD
James Heaton, PhD
Associate Investigator, Mass General Voice Center
Associate Professor of Surgery, Harvard Medical School
Adjunct Professor, MGH Institute of Health Professions

Tiffiny A. Hron, MD
Laryngeal Surgeon, Mass General Voice Center
 Nelson Roy, PhD
Nelson Roy, PhD
Professor of Communication Science and Disorder, University of Utah
 Lauren Tracy, MD
Lauren Tracy, MD
Laryngeal Surgeon, Boston Medical Center
Assistant Professor of Otolaryngology, Chobanian and Avedisian School of Medicine, Boston University
 Emma Willis, MS
Emma Willis, MS
Research Speech-Language Pathologist, Mass General Voice Center
PhD Student, Speech-Language Pathology, MGH Institute of Health Professions
 Jeremy Wolfberg, MS, CCC-SLP
Jeremy Wolfberg, MS, CCC-SLP
Research Speech-Language Pathologist, Mass General Voice Center
PhD Student, Speech-Language Pathology, MGH Institute of Health Professions
 Zilan Zhu
Zilan Zhu
MS Student, Speech-Language Pathology, MGH Institute of Health Professions
PROJECT 2 (LEAD: BOSTON UNIVERSITY)

Cara Stepp, PhD
Principal Investigator, Project 2, Vocal Hyperfunction Clinical Research Center at Mass General
Director, Sensorimotor Rehabilitation Engineering Lab, Boston University
Professor, Departments of Speech, Language & Hearing Sciences, Otolaryngology-Head & Neck Surgery, and Biomedical Engineering, Boston University

Allison Aaron, MS, CCC-SLP
Doctoral student, Sensorimotor Rehabilitation Engineering Lab,
Department of Speech, Language, and Hearing Sciences, Boston University
 Daniel Buckley, MS, CCC-SLP
Daniel Buckley, MS, CCC-SLP
Faculty Lecturer, Department of Speech, Language & Hearing Sciences, Boston University
 Megan Cushman, BS
Megan Cushman, BS
Research Coordinator and Lab Manager, STEPP Lab for Sensorimotor Rehabilitation Engineering, Speech, Language & Hearing Sciences, Boston University
 Kimberly Dahl, MS, CCC-SLP
Kimberly Dahl, MS, CCC-SLP
Doctoral Student, Sensorimotor Rehabilitation Engineering Lab, Department of Speech, Language, and Hearing Sciences, Boston University
 Manuel Díaz Cádiz, MS
Manuel Díaz Cádiz, MS
Research Fellow, Sensorimotor Rehabilitation Engineering Lab, Department of Speech, Language, and Hearing Sciences, Boston University
 Daria Dragicevic, BA
Daria Dragicevic, BA
Doctoral Student, Sensorimotor Rehabilitation Engineering Lab, Department of Speech, Language, and Hearing Sciences, Boston University
 Turley Duque
Turley Duque
Doctoral Student, Sensorimotor Rehabilitation Engineering Lab, Department of Speech, Language, and Hearing Sciences, Boston University
 Alex Estrada, BS
Alex Estrada, BS
Research Fellow, STEPP Lab for Sensorimotor Rehabilitation Engineering, Speech, Language & Hearing Sciences, Boston University
 Taylor Feaster, BA
Taylor Feaster, BA
Research Fellow, STEPP Lab for Sensorimotor Rehabilitation Engineering, Speech, Language & Hearing Sciences, Boston University
 Saul Frankford, PhD
Saul Frankford, PhD
Postdoctoral Fellow, STEPP Lab for Sensorimotor Rehabilitation Engineering, Speech, Language & Hearing Sciences, Boston University
 Nichole Houle, PhD, CCC-SLP
Nichole Houle, PhD, CCC-SLP
Postdoctoral Fellow, STEPP Lab for Sensorimotor Rehabilitation Engineering, Speech, Language & Hearing Sciences, Boston University
 Mara Kapsner-Smith, MS, CCC-SLP
Mara Kapsner-Smith, MS, CCC-SLP
PhD Student, Department of Speech and Hearing Sciences, University of Washington

Katherine Marks, PhD, CCC-SLP
Postdoctoral Research Fellow, Sensorimotor Rehabilitation Engineering Lab, Department of Speech, Language, and Hearing Sciences, Boston University

J. Pieter Noordzij, MD
Professor, Otolaryngology-Head & Neck Surgery, Boston University School of Medicine
 Joseph Perkell, PhD, DDS
Joseph Perkell, PhD, DDS
Senior Research Scientist, Department of Speech, Language & Hearing Sciences, Sargent College, Boston University
 Jose Manuel Rojas, BS
Jose Manuel Rojas, BS
Research Fellow, STEPP Lab for Sensorimotor Rehabilitation Engineering, Speech, Language & Hearing Sciences, Boston University
 Kaitlyn Siedman, BS
Kaitlyn Siedman, BS
 Nicole Tomassi, BS
Nicole Tomassi, BS
PhD Student, Stepp Lab for Sensorimotor Rehabilitation Engineering, Graduate Program for Neuroscience, Boston University
 Bridget Walsh, PhD, CCC-SLP
Bridget Walsh, PhD, CCC-SLP
Associate Professor, Communicative Sciences and Disorders, Michigan State University
 Hasini Weerathunge, BS
Hasini Weerathunge, BS
PhD Student, Stepp Lab for Sensorimotor Rehabilitation Engineering, Department of Biomedical Engineering, Boston University
PROJECT 3 (LEAD: UNIVERSIDAD TECNICA FEDERICO SANTA MARIA)

Matías Zañartu, PhD
Principal Investigator, Project 3, Vocal Hyperfunction Clinical Research Center at Mass General
Associate Professor, Department of Electronic Engineering, Universidad Técnica Federico Santa María

Byron Erath, PhD
Associate Professor, Department of Mechanical and Aeronautical Engineering, Clarkson University

Sean Peterson, PhD
Professor, Department of Mechanical and Mechatronics Engineering, University of Waterloo

Frank Guenther, PhD
Professor, Department of Speech, Language & Hearing Sciences, Boston University
Professor, Department of Biomedical Engineering, Boston University
 Preeti Sivasankar, PhD, CCC-SLP
Preeti Sivasankar, PhD, CCC-SLP
Professor and Department Head, Department of Speech, Language, and Hearing Sciences
Adjunct Faculty, Indiana University School of Medicine-West Lafayette

Gabriel Alzamendi, PhD
Assistant Research/Instructor Professor, Institute for Research and Development on Bioengineering and Bioinformatics, Universidad Nacional de Entre Ríos

Ali Bizhanpour
MS Student, Department of Mechanical and Aeronautical Engineering, Clarkson University

Carlos Calvache
PhD Student, Faculty of Basic and Applied Sciences, Universidad Militar Nueva Granada

Juan Pablo Cortés, PhD
Post-Doctoral Research Associate, Advanced Center for Electrical and Electronic Engineering, Universidad Técnica Federico Santa María

Jhosmary Cuadros, MS
PhD Student, Department of Electronic Engineering, Universidad Técnica Federico Santa María
 Jonathan Deng, MS, PhD
Jonathan Deng, MS, PhD
Post-Doctoral Research Associate, Department of Mechanical and Mechatronics Engineering, University of Waterloo
 Nicholas Hewko
Nicholas Hewko
PhD Student, Department of Electronic Engineering, Universidad Técnica Federico Santa María
 Emiro Ibarra, MS
Emiro Ibarra, MS
PhD Student, Department of Electronic Engineering, Universidad Técnica Federico Santa María
 Josué Martinez, MS
Josué Martinez, MS
PhD Student, Department of Electronic Engineering, Universidad Técnica Federico Santa María
 Rocío Ortega
Rocío Ortega
MS Student, Department of Electronic Engineering, Universidad Técnica Federico Santa María
 Jesus Parra, MS
Jesus Parra, MS
PhD Student, Department of Electronic Engineering, Universidad Técnica Federico Santa María
 Nicolás Quinteros
Nicolás Quinteros
PhD Student, Department of Electronic Engineering, Universidad Técnica Federico Santa María
 Trystan Semmens
Trystan Semmens
MS Student, Department of Mechanical and Mechatronics Engineering, University of Waterloo

Lucia Zepeda
Research Fellow, Advanced Center for Electrical and Electronic Engineering, Universidad Técnica Federico Santa María
PROJECT 4 (LEAD: MASS GENERAL)
 Jarrad Van Stan, MS, CCC-SLP
Jarrad Van Stan, MS, CCC-SLP
Principal Investigator, Project 4, Vocal Hyperfunction Clinical Research Center
Research Speech-Language Pathologist, Mass General Voice Center
Assistant Professor in Surgery, Harvard Medical School
Adjunct Assistant Professor, MGH Institute of Health Professions
 Robert Hillman, PhD, CCC-SLP
Robert Hillman, PhD, CCC-SLP
Co-Director and Research Director, Mass General Voice Center
Professor of Surgery, Harvard Medical School
Director of Research Programs, MGH Institute of Health Professions
 Grace Chow, BS
Grace Chow, BS
Clinical Research Coordinator, Boston Medical Center
 Jameson Cooper, MS, CCC-SLP
Jameson Cooper, MS, CCC-SLP
Research Speech-Language Pathologist, Mass General Voice Center
 Amanda Gillespie, PhD, CCC-SLP
Amanda Gillespie, PhD, CCC-SLP
Director of Speech Pathology and Co-Director, Emory Voice Center
Assistant Professor of Otolaryngology, Emory University School of Medicine
 Amy Gottlieb, MS-CF-SLP
Amy Gottlieb, MS-CF-SLP
Speech-Language Pathologist, Boston Medical Center

Dagmar Sternad, PhD
Professor of Biology, Electrical and Computer Engineering, and Physics, Northeastern University
 Lauren Tracy, MD
Lauren Tracy, MD
Laryngeal Surgeon, Boston Medical Center
Assistant Professor of Otolaryngology, Chobanian and Avedisian School of Medicine, Boston University
 Emma Willis, MS
Emma Willis, MS
Research Speech-Language Pathologist, Mass General Voice Center
PhD Student, Speech-Language Pathology, MGH Institute of Health Professions
 Jeremy Wolfberg, MS, CCC-SLP
Jeremy Wolfberg, MS, CCC-SLP
Research Speech-Language Pathologist, Mass General Voice Center
PhD Student, Speech-Language Pathology, MGH Institute of Health Professions
VHCRC Alumni

Defne Abur, BS
Assistant Professor, University of Groningen
 Lindsay Baron
Lindsay Baron
Former MS Student, Speech-Language Pathology, MGH Institute of Health Professions

James Burns, MD
Former Associate Visiting Surgeon, Mass General Voice Center
 Tamara Carrera
Tamara Carrera
Undergraduate Student, Department of Electronic Engineering, Universidad Técnica Federico Santa María

Christian Castro, SLP
Research Fellow, Advanced Center for Electrical and Electronic Engineering, Universidad Técnica Federico Santa María
 Harold Cheyne II, PhD
Harold Cheyne II, PhD
Manager of Audio Systems Research, Bose Corporation

Gregory Ciccarelli, PhD
Amazon.com, Inc.
 Joseph Deauna
Joseph Deauna
SLP Clinical Fellow, Spaulding Outpatient Center Cambridge
 Anton Dolling, BA
Anton Dolling, BA
Content Strategist, Ally
 Sarah Eastman, MS
Sarah Eastman, MS
Singing Voice Specialist and Speech-Language Pathology Clinical Fellow, the Voice Rehab, Sunrise (Miami), FL

Víctor Espinoza, PhD
Research Fellow, Department of Sound, Universidad de Chile

Gabriel Galindo, PhD
Formerly with the Department of Electronic Engineering, Universidad Técnica Federico Santa María
 Kayla Gautereaux
Kayla Gautereaux
Associate Professor, Boston Conservatory at Berklee

Elizabeth Heller Murray, PhD, CCC-SLP
Assistant Professor, Department of Communication Sciences and Disorders, Temple University
 Javier González, MS
Javier González, MS
PhD Student, Department of Electronic Engineering, Universidad Técnica Federico Santa María
 Jose Javier Gonzalez Ortiz
Jose Javier Gonzalez Ortiz
PhD Student, Electrical Engineering and Computer Science, Massachusetts Institute of Technology
 Paul J. Hadwin, PhD
Paul J. Hadwin, PhD
Post-Doctoral Research Associate, Department of Mechanical and Mechatronics Engineering, University of Waterloo
 Liane Houde, MS
Liane Houde, MS
Former MS Student, Speech-Language Pathology, MGH Institute of Health Professions
Chuanbing Huo, MS
Former MS Student, Speech-Language Pathology, MGH Institute of Health Professions
 Samantha Kridgen, MS
Samantha Kridgen, MS
Speech-Language Pathology Clinical Fellow, University of Alabama at Birmingham

Rodrigo Manriquez, MS
Research Fellow, Advanced Center for Electrical and Electronic Engineering, Universidad Técnica Federico Santa María
 Mohsen Motie-Shirazi, MS
Mohsen Motie-Shirazi, MS
Former PhD Student, Department of Mechanical and Aeronautical Engineering, Clarkson University

Juan Mucarquer, MS
Formerly with the Department of Electronic Engineering, Universidad Técnica Federico Santa María
 Charlie Nudelman, MS
Charlie Nudelman, MS
Voice Pathologist Clinical Fellow, Lakeshore Professional Voice Center, St. Clair Shores, MI
 Benjamin Opazo, BS
Benjamin Opazo, BS
MS Student, Department of Electronic Engineering, Universidad Técnica Federico Santa María

Yeonggwang Park, PhD
Postdoctoral Fellow, Department of Communication Science and Disorders, University of South Florida

Pavel Prado, PhD
Post-Doctoral Research Associate, Advanced Center for Electrical and Electronic Engineering, Universidad Técnica Federico Santa María

Thomas Quatieri, PhD
Senior Staff, Human Health and Performance Systems Group, MIT Lincoln Laboratory
 Javier Romero, MS
Javier Romero, MS
Formerly with the Department of Electronic Engineering, Universidad Técnica Federico Santa María
 Roxanne Segina, BA
Roxanne Segina, BA
Former MS Student, Stepp Lab for Sensorimotor Rehabilitation Engineering, Department of Speech, Language, & Hearing Sciences, Boston University
 Ariana Seidman, MS
Ariana Seidman, MS
Speech Language Pathology Clinical Fellow, Ochsner LSU Health Shreveport
 Mohamed Serry, MS
Mohamed Serry, MS
PhD Student, Department of Mechanical and Mechatronics Engineering, University of Waterloo
 Joseph Stemple, PhD
Joseph Stemple, PhD
Professor of Rehabilitation Science and Otolaryngology, University of Kentucky
Co-Director, Laryngeal and Speech Dynamics Laboratory, University of Kentucky
 Austeja Subaciute, BS
Austeja Subaciute, BS

Laura Toles, PhD, CCC-SLP
Assistant Professor, Department of Otolaryngology-Head and Neck Surgery,
University of Texas Southwestern Medical Center
 Mark Vangel, PhD
Mark Vangel, PhD
Statistician, Mass General Hospital
Assistant Professor in Radiology, Harvard Medical School
Biostatistician, General Clinical Research Center, Massachusetts Institute of Technology
 Alessandra Verdi, MS
Alessandra Verdi, MS
Clinical Fellow, Emory Healthcare, Atlanta, GA

Thomas Whittico, MS
Former MS student, Speech-Language Pathology, MGH Institute of Health Professions
 Brianna Williams, MS, CCC-SLP
Brianna Williams, MS, CCC-SLP
Speech-Language Pathologist, Northside Hospital, Atlanta, GA

Oliver Saunders Wilder, PhD
Post-Doctoral Fellow, Media Lab and Simons Center for the Social Brain, Massachusetts Institute of Technology

Juan Yuz, PhD
Professor, Department of Electronic Engineering, Universidad Técnica Federico Santa María
Learn More
The Vocal Hyperfunction Clinical Research Center explores methods and technologies to prevent, diagnose and treat vocal hyperfunction, which is associated with the most frequently occurring types of voice disorders.
