NewsJul | 11 | 2024
Study Finds That Tennessee’s Shift in HIV Prevention Funding Will Lead to Poorer Health Outcomes for its Residents
 BOSTON – A recent study in Clinical Infectious Diseases led by Massachusetts General Hospital investigators, warns that Tennessee's new HIV prevention funding policy will lead to poorer health outcomes for its residents.
BOSTON – A recent study in Clinical Infectious Diseases led by Massachusetts General Hospital investigators, warns that Tennessee's new HIV prevention funding policy will lead to poorer health outcomes for its residents.
Tennessee plans to reject $6 million in Centers for Disease Control and Prevention (CDC) funding. Instead, they'll redirect state resources for HIV prevention to first responders, pregnant individuals and survivors of sex trafficking.
Using a microsimulation model, a team of researchers led by Ethan Borre, MD, PhD, found that the shift in funding will harm high-risk groups while providing only minimal benefits for new priority populations.
CDC HIV prevention funding has prevented countless HIV cases and deaths in Tennessee, and throughout the United States, especially amongst those at highest risk for HIV, including men who have sex with men, transgender women and heterosexual Black women. Rejecting this funding puts lives at risk.
Ethan Borre, MD, PhD
Department of Medicine
Teaming up with Tennessee-based community organizations Nashville CARES and Friends For All Memphis (recipients of the CDC funding), as well as investigators from Vanderbilt University, Yale University, and the national HIV Medicine Association, Drs. Borre, Neilan, and colleagues used an MGH-based and widely cited microsimulation model to assess the potential effects of HIV prevention funding reallocation in Tennessee.
The analysis revealed that reallocating HIV prevention funding away from CDC-prioritized populations (men who have sex with men, transgender women, and heterosexual Black women) towards Tennessee-prioritized populations (first responders, pregnant people, and survivors of sex trafficking) would result in additional HIV transmissions and deaths.
“Shifting funds from those at higher risk to those at lower risk will harm individuals, curb efforts to combat the HIV epidemic, and strain the state’s budget,” says senior author Anne Neilan, MD, MPH, an investigator in the Division of Infectious Disease at Massachusetts General Hospital. “Tennessee's new HIV prevention funding policy will lead to 166 additional HIV transmissions, 190 additional deaths, and 843 life-years lost over 10 years.”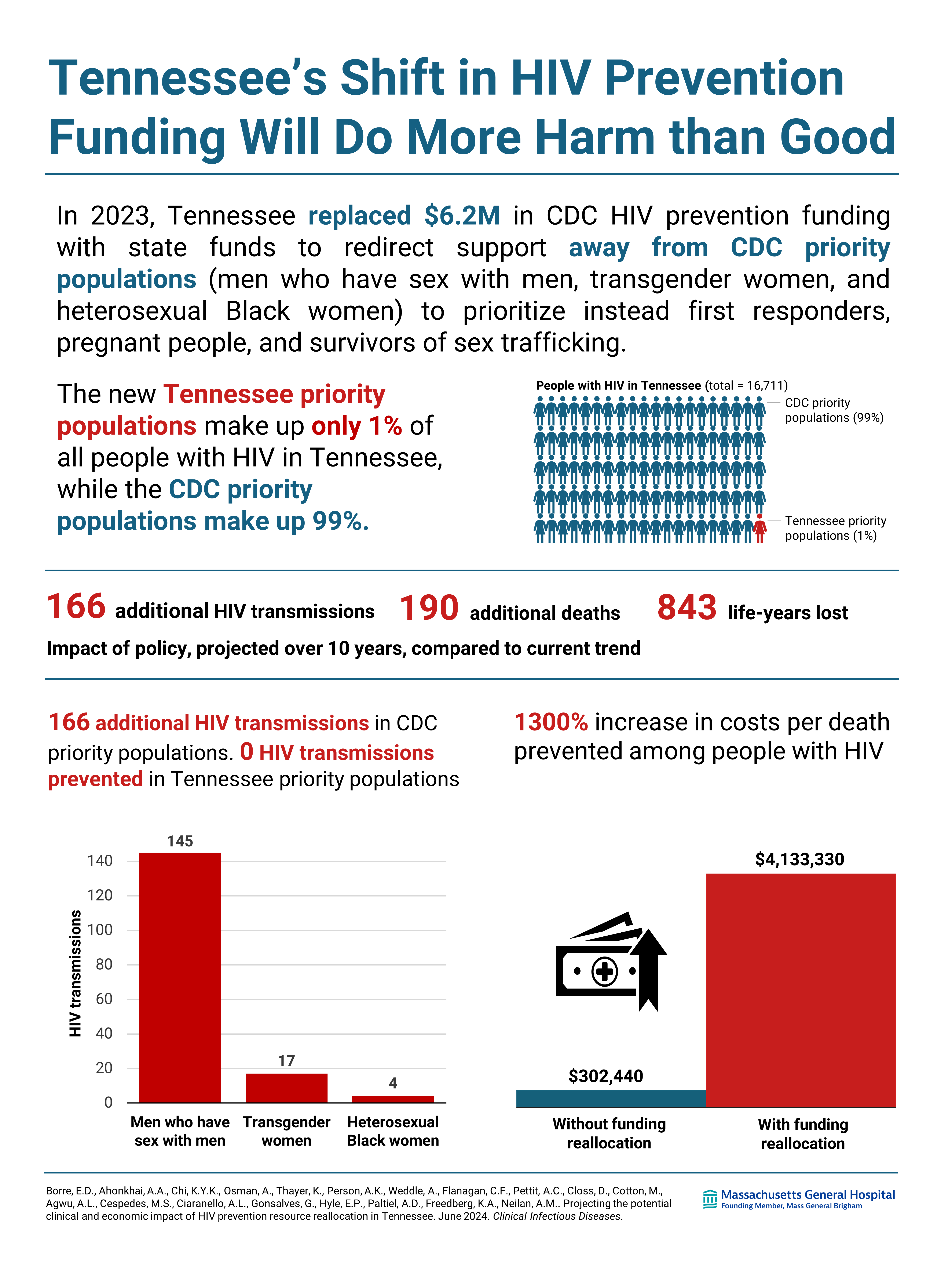
“The proposed changes in funding will have wide-reaching effects on community-based organizations who provide HIV prevention services directly to Tennesseeans. We in the community are very concerned about the effects of funding losses on our day-to-day operations and the people we serve,” adds Amna Osman, MPA, co-author and Chief Executive Officer of Nashville CARES.
Tennessee community leaders also have concerns around the equity of the proposed funding reallocation. Mia Cotton, MPH, co-author and Chief Program Officer at Friends For All Memphis notes, “Tennessee is already seeing serious disparities in HIV outcomes among racial and gender minorities, particularly amongst Black Tennesseans and transgender women.
Our findings suggest that the new funding policy would worsen existing disparities, with minoritized populations experiencing a lion’s share of the increased deaths.”
Mia Cotton, MPH
Chief Program Officer, Friends for All Memphis
Author Info
Neilan is also an Assistant Professor in Pediatrics and Medicine at Harvard Medical School, and Borre is an Internal Medicine Resident at Massachusetts General Hospital. Additional co-authors of the report are Aima A. Ahonkhai, MD, MPH, Kyu-young Kevin Chi, BA, Andrea L. Ciaranello, MD, MPH, Emily P. Hyle, MD, MSc, Clare F. Flanagan, MPH, Kenneth A. Freedberg, MD, MSc, MGH Medical Practice Evaluation Center; Krista Thayer, MS, David Closs, BA, Mia Cotton, MPH, Friends For All Memphis; Anna K. Person, MD, April C. Pettit, MD, MPH, Division of Infectious Diseases, Department of Medicine, Vanderbilt University Medical Center Gregg Gonsalves, PhD, A. David Paltiel, PhD, Public Health Modeling Unit and Department of Health Policy and Management, Yale School of Public Health; Allison L. Agwu, MD, ScM, Division of Infectious Diseases, Department of Medicine, Johns Hopkins University School of Medicine; Michelle S. Cespedes, MD, MS, Division of Infectious Diseases, Department of Medicine, Icahn School of Medicine at Mount Sinai; Andrea Weddle, MSW, the HIV Medicine Association of the Infectious Diseases Society of America.
Funding
This work was supported by the Eunice Kennedy Shriver National Institute for Child Health and Human Development, the National Institute of Allergy and Infectious Diseases, the National Institute on Drug Abuse, and the National Institute of Mental Health of the National Institutes of Health. The study received additional funding from the MGH Department of Medicine Transformative Scholar Award, the MGH Jerome and Celia Reich Endowed Scholar Award, and the MGH James and Audrey Foster Research Scholar Award of the MGH Executive Committee on Research, and the Ryan White Care Act Part A and the End the HIV Epidemic to DC.
Paper Cited:
Borre, E. D., Ahonkhai, A. A., Chi, K. K., Osman, A., Thayer, K., Person, A. K., Weddle, A., Flanagan, C. F., Pettit, A. C., Closs, D., Cotton, M., Agwu, A. L., Cespedes, M. S., Ciaranello, A. L., Gonsalves, G., Hyle, E. P., Paltiel, A. D., Freedberg, K. A., & Neilan, A. M. (2024). Projecting the Potential Clinical and Economic Impact of Human Immunodeficiency Virus Prevention Resource Reallocation in Tennessee. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America, ciae243. Advance online publication. https://doi.org/10.1093/cid/ciae243
-
![]()
- Infectious Diseases
- Department of Medicine
Type
Centers and Departments
Topics
Check out the Mass General Research Institute blog
Bench Press highlights the groundbreaking research and boundary-pushing scientists working to improve human health and fight disease.
Support Research at Mass General
Your gift helps fund groundbreaking research aimed at understanding, treating and preventing human disease.
About Massachusetts General Hospital
Massachusetts General Hospital, founded in 1811, is the original and largest teaching hospital of Harvard Medical School. The Mass General Research Institute conducts the largest hospital-based research program in the nation, with annual research operations of more than $1 billion and comprises more than 9,500 researchers working across more than 30 institutes, centers and departments. MGH is a founding member of the Mass General Brigham healthcare system.

