Clinical Trial Reveals Benefits of Inhaled Nitric Oxide for Patients with Respiratory Failure Due to COVID-19 Pneumonia
Treatment improved blood oxygen levels and lowered the risk of long-term sensory and motor neurologic symptoms.
Staff StoryMay | 28 | 2020

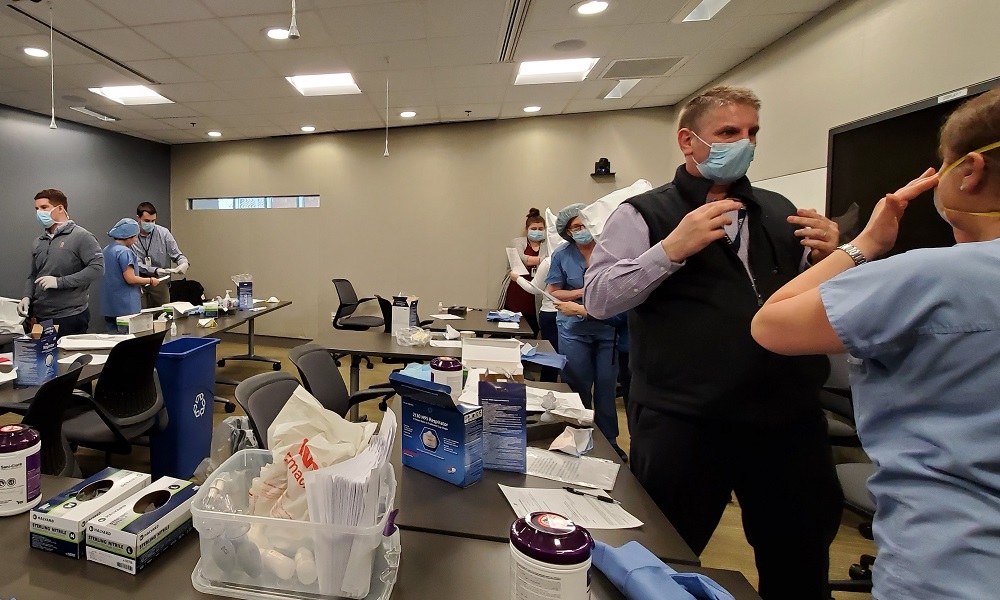
Fit testing Massachusetts General Hospital staff for proper N95 respirator use is a challenging process even in the best of times. When compounded with a greatly enhanced, pandemic-related demand and severe global N95 supply issues, it calls for a staggering amount of flexibility and teamwork.
The Mass General Environmental Health and Safety Department has led a recent hospitalwide collaboration to meet this weighty challenge. This includes Paula Lyons, the department’s staff assistant, who to date has electronically documented more than 6,200 fit test records via Red Cap over the course of the fit testing crush. Many staff needed to wear respirators for the first time and—due to the shortages of the N95s typically used at the hospital—many employees had to be re-fitted for alternate models to help preserve supplies.

“It was our obligation to step up and make sure we did everything we could to make sure our hospital staff was comfortable, safe and secure in their respiratory protection,” says Bob Castaldo, director of Environmental Health and Safety.
After 10 clinical floors were designated as units to care for patients with COVID-19 in mid-March, Castaldo and his team quickly assessed the massive job ahead of them. "It took us until the first week of April to finish those 10 floors and fit almost 1,200 people in a couple of weeks,” says Castaldo, who had the help of trained fit testers on those units. “That is the number we'd normally do in about a year.”
It often takes several tries with various models and sizes to provide the proper respirator, adding to the number of actual tests that need to be carried out. “This crisis highlighted for our staff the value of this rigorous, annually-required fit testing,” says Anne Sallee, biosafety manager.
In early April, the team switched tactics and set up an open-to-all central fitting station in the East Garden Room on the main campus. Their busiest day was April 9, Castaldo says, when department staff—in collaboration with fit testers from Perioperative Services and Physical Therapy—fitted more than 750 people. “We were under siege! Lines wrapped down the hallway and around toward the cafeteria entrance, with a two-hour wait for some staff.”
The Environmental Health and Safety team continued trainings in April and May, which included fitting staff at off-site locations. “Our goal was to decentralize as much as possible, and provide our experience and expertise as needed,” says Castaldo.
Bob CastaldoIt was our obligation to step up and make sure we did everything we could to make sure our hospital staff was comfortable, safe and secure in their respiratory protection.
While addressing clinical staff needs, the central station also was available to fit test the reprocessed N95s from the Battelle System. “There’s been lots of publicity about the reprocessing of N95 respirators. When they come back to us, we have to ensure their continued quality,” says Castaldo. “Samples out of those reprocessed respirators are re-tested to make sure they’re still fitting safely. Our unit-based fit testers on the floors did a lot of that work.”
Stressing the importance of hospitalwide collaboration, Castaldo highlighted the contributions from all corners, including the Emergency Department, the Biothreats Response Team and Information Services. In addition, Castaldo says Mass General Pharmacy was quick to respond when the group needed assistance. “When we ran out of the saccharin solution we need to carry out testing, our Pharmacy colleagues were able to make both the sensitivity and testing solutions we need. When the Boston Police Department also ran out of these materials and reached out to us for help, we were able to provide them with some of our supply.”
Castaldo says while the training was a massive undertaking, it was well worth the workload. “At the end of the day, what really drove everybody was our staff’s safety. We saw a lot of anxiety related to N95 usage, but we also saw many people leaving the central station with a sense of confidence in the equipment.”
Adds Sallee, “Our staff’s safety was being assured. Everyone rolled up their sleeves and got the job done. It's a testament to the whole MGH family that we were all able to get as much done in that short amount of time."
Treatment improved blood oxygen levels and lowered the risk of long-term sensory and motor neurologic symptoms.
Results indicate a link between reduced mobility during the pandemic and greater risk for depressive symptoms.
In surveys completed throughout the COVID-19 pandemic by U.S. adults, trust in physicians and hospitals decreased over time in every socioeconomic group.
BCG-treated individuals had a significantly lower rate of COVID-19 infection compared with the placebo group and a significantly lower rate of infectious diseases overall.
Researchers found that a person with a diagnosis of Down syndrome and COVID-19 pneumonia had six times the odds of having a Do Not Resuscitate (DNR) status ordered at hospital admission.
Aram J. Krauson, PhD, of the Department of Pathology at Mass General, is the first author and James Stone, MD, PhD, is the senior author of a new study in NPJ Vaccines, Duration of SARS-CoV-2 mRNA Vaccine Persistence and Factors Associated with Cardiac Involvement in Recently Vaccinated Patients.
Treatment improved blood oxygen levels and lowered the risk of long-term sensory and motor neurologic symptoms.
Results indicate a link between reduced mobility during the pandemic and greater risk for depressive symptoms.
In surveys completed throughout the COVID-19 pandemic by U.S. adults, trust in physicians and hospitals decreased over time in every socioeconomic group.
BCG-treated individuals had a significantly lower rate of COVID-19 infection compared with the placebo group and a significantly lower rate of infectious diseases overall.